- Home
- Education & Events
- Conference Archive
2023 Schedule
2023 Conference ScheduleConference Schedule(subject to change) Nursing CEThis conference is approved for Nursing CE through the California Board of Nursing. |
TimeCentral time zone |
Saturday, Oct 28
|
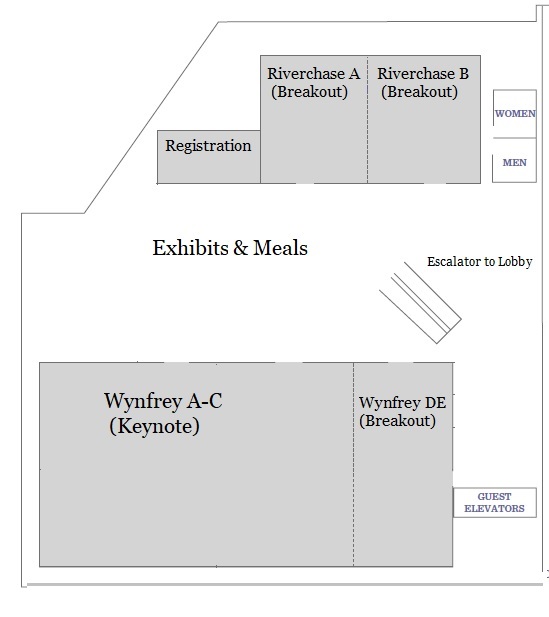
Location |
| 8am - 11am |
Pre-Conference Workshops (separate registration fee required) |
Riverchase A & B |
| 8am - 12pm |
Exhibit Area Setup |
2nd Level Foyer |
| 11am - 3:15pm |
Registration |
2nd Level Foyer |
| 11 - 12pm |
First Time Attendee & New Member Orientation |
Wynfrey ABC |
| 12pm - 4:30pm |
Exhibit Area |
2nd Level Foyer |
| 12pm - 1pm |
Welcome Lunch (open to all attendees) |
Wynfrey ABC |
| 1pm - 2pm |
Keynote Address
This presentation will focus on emerging trends in leadership that underscore the need for leaders to prioritize diversity, equity, equality and inclusion. Leaders must create work environments that promote safety, fairness and justice for all staff. This presentation will highlight the role of organizational justice and why it is important for nurse leaders to use social justice lens to address workforce issues such as unequal pay, unfair promotions and non-inclusive work environments.
|
Wynfrey ABC |
| 2:10pm - 3:00pm |
Breakout 1 10-ASP. Preparing international nurse researchers: an equitable and inclusive PhD program initiative
Learner Objectives:
48-EBP. Enhancing Nursing Global Health Competencies of Undergraduate Nursing Students through A Study Abroad Experience "Down Under"
Learner Objectives:
|
Riverchase A |
| 2:10pm - 3:00pm |
Breakout 2 21-R. Examining Moral Injury, Well-being, Resilience, and their impact on Nurse Leaders' Intentions to Leave Position or Profession Amid COVID-19 Pandemic
Learner Objectives:
80-R. Using a Measure of Nurse Manager Reasons for Leaving to Inform Role Transformation for the Future
Learner Objectives:
|
Riverchase B |
| 2:10pm - 3:00pm |
Breakout 3 60-R. Factors Influencing Direct Care Nurses Intent to Leave and Implications for Retention
Learner Objectives:
53-QI. Virtual Nurses: Investing Intellectual Human Capital
Learner Objectives:
|
Wynfrey DE |
| 3:10pm - 4:00pm |
Breakout 4 23-QI. Empowering nurse leaders to re-think and re-engineer the practice environment through the use of a conceptual framework for nurse retention
Learner Objectives:
28-EBP. Cultural Intelligence: Honoring the Shared Human Experience Through Human-Centered Leadership
Learner Objectives:
|
Riverchase A |
| 3:10pm - 4:00pm |
Breakout 5 34-QI. Are We Measuring Our EDI performance? That is the Question for "U"CLA
Learner Objectives:
9-R. Does Zip Code Predict Patient Outcomes?
Learner Objectives:
|
Riverchase B |
| 3:10pm - 4:00pm |
Breakout 6 22-R. Incivility and the Impact of Nurse Leader Styles and Characteristics
Learner Objectives:
5-R. Retelling the Stories: Registered Nurses’ Lived Experiences of Peer-to-Peer Incivility in the Workplace
Learner Objectives:
|
Wynfrey DE |
|
4:45pm - 7:30pm |
Welcome Reception hosted by the This event is open to all attendees Transportation: |
|
Poster Presentations
Sunday, 12pm - 1:50pm, ordered by Abstract ID
- Debra Hampton, PhD, MSN, RN, NEA-BC, CENP, FACHE, FAONL; UK College of Nursing; Lexington, Kentucky
To illustrate a model that can be used to describe the levels/aspects of competency. To present examples of assignments that can be used in a leadership course to validate competency. To begin to demystify the challenge of validating competency for the advanced level 2021 AACN Essentials.
8-R. COVID-Related Burnout: Nurses' Perspectives and Priorities
- Roberta Kaplow, Ph.D., APRN-CCNS, AOCNS, CCRN, FAAN; Emory University Hospital; Atlanta, Georgia
- Polly Willis, MSN, NE-BC, PCCN; Emory University Hospital; Atlanta, Georgia
- Dinah Steele, DNP, RN, CMSRN; Emory St. Josephs Hospital; Atlanta, Georgia
Describe the degree of burnout experienced by nurses during the pandemic List the priority interventions recommended by nurses to promote clinician wellbeing.
- Kathleen Diatta, PhD, RN, NE-BC; Emory University Hospital; Atlanta, Georgia
- David Reinhart, DNP, MBA, RN, CNOR; Atlanta, Georgia
- Stacie Roberts, MSN, RN; Emory University Hospital; Atlanta, Georgia
Describe the rationale for developing a PACU Nurse Residency Program Apply strategies to develop a nurse residency program at other facilities
- Todd Tussing, DNP, RN, CENP, NEA-BC; The Ohio State University; Columbus, Ohio
- Angie Blevins, RP, OSBA, CPHRM; Wexner Medical Center at The Ohio State University; Columbus, Ohio
- Julia Turner, JD, MBA, BSN, CPHRM; University of California San Francisco; San Francisco, California
- Brett Hagenbuch, MHA, BSN, RN, NE-BC; The James Cancer Hospital at The Ohio State University; Columbus, Ohio
Participant will be able to describe Leadership WalkRounds and the evidence supporting its use. Participant will be able to design a Leadership WalkRounds process for Implementation.
27-EBP. Strategic Planning: Moving from Plan to Implementation
- Teresa Welch, EdD, MSN, RN, NEA-BC; The University of Alabama; Tuscaloosa, Alabama
- Todd Smith, PhD, MBA, MSHA, RN, NEA-BC; The University of Alabama; Tuscaloosa, Alabama
Discuss implementation science. Differentiate between strategic plan, strategic management, strategic decision-making, and strategic implementation. Identify key implementation strategies espoused by implementation science research for successful change management.
31-ASP. Clinical Scholars Program: Building leadership capacity through an academic-clinical partnership
- Tedra Smith, DNP, CRNP, CPNP-PC, CNE, CHSE; University of Alabama at Birmingham; Birmingham, Alabama
- Curry Bordelon, DNP, MBA, NNP-BC, CPNP-AC, CNE; University of Alabama at Birmingham; Birmingham, Alabama
Describe the benefits of an academic-clinical partnership to build leadership capacity among staff nurses. Discuss the effectiveness of a structured program to amplify the ability to design, implement, and evaluate quality improvement initiatives.
 |
32-QI. Cultivating Organizational Change Toward Cultural Awareness in Nurses Through Continued Education
- Kemi Reeves, MSN, RN, GNP-BC; UCLA Health; Los Angeles, California
Describe the development of a quality improvement project aimed to impact the cultural awareness and adherence to health system policies addressing discrimination. Appraise organizational efforts to building a culture of care and inclusivity as a means to foster wellness, staff retention, and grow a diverse nurse workforce.
35-EBP. Expanding Stakeholder Access, While Protecting Your Intellectual Property Rights: Developing and Disseminating Evidence-Based Resources to Support Leadership Practice.
- Joy Parchment, PhD, RN, NEA-BC, CPDC; University of Central Florida; Orlando, Florida
- Sandra Galura, PhD, RN; University of Central Florida; Orlando, Florida
Describe steps to develop an evidence-based resource to support frontline nurse leaders. Discuss options for disseminating developed leadership resources to key practice stakeholders. Explain necessary actions to protect intellectual property rights.
37-R. COVID-19 Pandemic Response Implementation and the Impact on the Work Environments of Brazilian Intensive Care Units
- Liana Amorim Correa Trotte, Assistant Professor; Universidade Federal do Rio de Janeiro; Brazil
- José Luis Guedes Santos, Assistant Professor; Universidade Federal de Santa Catarina; Brazil
- Alacoque Lorenzin Erdmann, Full Professor; Universidade Federal de Santa Catarina; Rio de Janeiro, Brazil
- Maria Aparecida Pereira Dos Santos Santana, RN; Universidade Federal do Rio de Janeiro; Brazil
- Marluci Andrade Conceição Stipp, Full Professor; Universidade Federal do Rio de Janeiro, Brazil
To contribute to performing positive nursing practice environments can significantly improve patient care, nursing staff satisfaction, and overall health outcomes To evaluate effective nursing coordination and leadership to sustain a healthy work environment, especially when faced with challenging circumstances and resource constraints.
38-R. Mapping of terminal hygiene of intensive care beds using Lean Healthcare tools
- Marluci Andrade Conceição Stipp, Full Professor; Universidade Federal do Rio de Janeiro; Brazil
- Joana de Oliveira Pantoja Freire, Registered Nurse; Universidade Federal do Rio de Janeiro; Brazil
- Christiany Moçali Gonzalez, Registered Nurse; Universidade Federal do Rio de Janeiro; Brazil
- Graciele Oroski Paes, Associate Professor; Universidade Federal do Rio de Janeiro; Brazil
- Liana Amorim Correa Trotte, Assistant Professor; Universidade Federal do Rio de Janeiro, Brazil
To create of a Cleaning quality indicator To map of the technique and direction of movements on different surfaces To estabilish a percentage of completely and correctly cleaned surfaces
40-QI. Oral Health: Addressing Equity and Inclusion to Evade Variations in Patient Care
**Cannot attend in person**
- Anila Ladak, DNP, RN, CNS, GNP-BC; UCLA; Los Angeles, California
- Stephanie Jackson, DNP, MSN, RN, AOCNS, BMTCN; UCLA; Los Angeles, California
Describe the significance of the problem and current evidence to support practice change. Review the quality improvement process for improving the oral health across all ages and population groups in health system. Appraise the outcomes and future considerations of the quality improvement initiative. Discuss the implications of the project in building leaders for an equitable and inclusive future.
- K. David Bailey, PhD, MBA, RN, CCRN-K, NEA-BC, FACHE, FAAN; UCLA Health - Santa Monica Medical Center; Santa Monica, California
Explore how relational leader styles influence patient, nurse, and organizational outcomes. Differentiate how the various relational leadership styles influence healthy work environments and RN satisfaction. Explain how the various relational leadership styles affect patient outcomes and satisfaction.
43-EBP. Building capacity for mentoring through educating nurse leaders
- Annette Harrilson, RN, MSN, DNP; Piedmont Fayette Hospital; Fayetteville, Georgia
- Margot (Lisa) Hedenstrom, PhD, RN, MSN, MBA, NEA-BC; Kennesaw State University; Kennesaw, Georgia
At the end of this presentation, the participants will be able to outline the components and describe an educational intervention for nurse leaders to help increase knowledge and awareness of nurse leaders on mentoring. At the end of the presentation, the participants will be able to identify the potential benefits of a mentoring education program to build nurse leader capacity to strengthen diversity and inclusion in the workforce.
- Patricia A. Patrician, PhD, RN, FAAN; University of Alabama at Birmingham; Birmingham, Alabama
- Aoyjai P. Montgomery, PhD, BSN; University of Alabama at Birmingham; Birmingham, Alabama
- Katherine A. Meese, PhD; University of Alabama at Birmingham; Birmingham, Alabama
- Allyson G. Hall, PhD, MBA, MHS; University of Alabama at Birmingham; Birmingham, Alabama
- Rebecca (Suzie) Miltner, PhD, RN, FAAN; University of Alabama at Birmingham; Alabama, Alabama
To identify the sources of distress among nurses and nurse leaders in the immediate post-pandemic timeframe. To understand the design and development of a nurse-led organizational intervention to improve well-being.
52-R. Emotional Exhaustion of nursing professionals coping with the Covid-19 pandemic: What has leadership learned?
- DANIELLE SARAIVA TUMA DOS REIS, Profa da Universidade Federal do Pará; Universidade Federal do Pará; Belém, Brazil
- Sara Socorro da Silva Silva, Bolsista de iniciação científica; Universidade Federal do Pará; Belém, Brazil
- Carlos Leonardo Figueiredo Cunha, Prof da Universidade Federal do Maranhão; Universidade Federal do Maranhão; São Luis, Brazil
- José Luis Guedes dos Santos, Professor da Universidade Federal de Santa Catarina; Universidade Federal de Santa Catarina; Florianópolis, Brazil
- Gabriela MARCELLINO DE MELO LANZONI, Professor da Universidade Federal de Santa Catarina; Universidade Federal de Santa Catarina, Brazil
Identify the challenges faced by nursing leadership in the Covid-19 pandemic regarding emotional exhaustion of nursing technicians according to the dimensions of Burnout Syndrome (BS). Show which work environments (wards, intensive care unit and emergency room) influenced the psychological health of nursing technicians during the pandemic. Correlate the working conditions of nursing technicians who provided care to patients with Covid-19 with the dimensions of Burnout Syndrome (BS).
54-R. Quality Matters: Nurse Staffing and Clinical Outcomes
- Shea Polancich; Birmingham, Alabama
- Tracey Dick; Birmingham, Alabama
- Terri Poe; Birmingham, Alabama Aoy Montgomery; Birmingham, Alabama
- Patricia Patrician; Alabama, Alabama
Participants will describe the critical elements for leading and sustaining positive nursing quality outcomes. Recognize barriers improving nursing outcomes during crisis.
57-QI. Learning Health Center Leadership Makes the Case for Quality in Reducing Hospital Acquired Pressure Injury
- Shea Polancich; Birmingham, Alabama
- Shannon Layton; Birmingham, Alabama
- Rebecca Miltner; Birmingham, Alabama
Participants will describe the critical elements for leading sustainable quality improvement efforts in a learning health center. Recognize barriers to sustainable improvement in a learning health center.
 |
58-R. The Impact of Span of Control on Nurse Managers and Hospital Outcomes
- Asiah Ruffin, BSN, RN; University of Alabama at Birmingham; Birmingham, Alabama
- Maria R. Shirey, PhD, MBA, RN, NEA-BC, ANEF, FACHE, FAAN; University of Alabama at Birmingham; Birmingham, Alabama
- Tracey Dick, PhD, RN, CNE, COI; University of Alabama at Birmingham; Birmingham, Alabama
- Pariya Fazeli, PhD; University of Alabama at Birmingham; Birmingham, Alabama
- Patricia A. Patrician, PhD, RN, FAAN; University of Alabama at Birmingham; Alabama, Alabama
To examine work-related factors associated with nurse manager span of control. To provide a comprehensive definition of nurse manager span of control.
62-ASP. Sustaining Patient Experience Care Transition Metrics: Leveraging Academic Practice Partnerships
- Shannon Layton, DNP, RN, LICSW, NEA-BC, CNL, CNE,; University of Alabama at Birmingham School of Nursing; Birmingham, Alabama
- Sylvia Britt, PhD, RN; Birmingham, Alabama Randy Moore, DNP, RN; United States Department of Veterans Affairs; Birmingham, Alabama
- Patricia Patrician, PhD, RN, FAAN; University of Alabama at Birmingham School of Nursing; Birmingham, Alabama
- Rebecca (Suzie) Miltner, PhD, RN, NEA-BC, FAAN; University of Alabama at Birmingham School of Nursing; Alabama, Alabama
Describe the benefits of leading diverse and inclusive quality improvement teams Articulate the value that leadership obtained by consulting a diverse and inclusive veteran stakeholder group when improving veteran patient experience. Illustrate the value of utilizing academic practice partnerships to create solutions for barriers encountered in quality improvement. Display the value of incorporating leadership opportunities for nurse residents into project sustainment.
63-ASP. Innovation Ignite! Preparing Nurse Leaders for engagement in Health Services Innovation
- Roberta Pawlak, PhD, RN, NEA-BC; University of Wisconsin - Madison; Madison, Wisconsin
Describe characteristics of innovation, and skills of innovative leaders. Identify resources to support nurse leader engagement in health service innovation. Personalize a plan for ‘next steps’ to ignite the innovator within!!
64-EBP. Leading Change: Moving from Quality Improvement to Research to ensure Scale-up and Spread of Evidence-based Practice
- Mary Dolansky, PhD, RN; Case Western Reserve University; Cleveland, Ohio
- Anne Pohnert, DNP, BSN, FNP-BC, RN; MinuteClinic CVS Enterprise; Woonsocket, Rhode Island
Discuss the role of leadership to drive quality improvement and implementation of science methods and strategies in implementing evidence-based practice into a national health system. Describe the results of the added benefit of using research methods to contribute to the spread and scale-up of the integration of evi
65-QI. Introduction of an Innovative Care-Based Delivery Model
- Tracey K. Dick, PhD, RN, CNE, COI; UAB School of Nursing; Birmingham, Alabama
- Jennifer H. Ledlow, MSN, RN, CCRN-K, CNL, CNE; UAB School of Nursing; Birmingham, Alabama
- Rebecca S. (Suzie) Miltner, PhD, RN, NEA-BC, FAAN; UAB School of Nursing; Birmingham, Alabama
- Keri Thomas, MSN, RN, FNP-C; UAB Hospital Nursing Services; Birmingham, Alabama
- Shea Polancich, PhD, RN, FAAN; UAB School of Nursing; Alabama, Alabama
Attendees will recognize the potential impact an innovative care-based delivery model of nursing care may have on employee satisfaction, retention, and overall patient care. Attendees will develop ideas on strategies for implementing innovative care-based delivery models of nursing care within their institutions.
 |
70-ASP. Who are nurse leaders? How do we know?
- Roberta Pawlak, PhD, RN, NEA-BC; University of Wisconsin - Madison; Madison, Wisconsin
Discuss the theoretical roots of nursing and determine how theory informs nursing as a practice discipline. Identify connections between mid-range and situation-specific theories with our professional standards in Nursing Leadership. Apply the “Letter to my future self” tool to bridge nursing theory to current and future nursing leadership practice.
71-ASP. Challenging assumptions in the quest for equitable maternal child health
- Candace Knight, PhD, RN, FAAN; University of Alabama at Birmingham School of Nursing; Birmingham, Alabama
- Charlotte Walton, RN, MPH; Birmingham, Alabama
- Haley Fenn, MS; Birmingham, Alabama
- Taishayla McKitt, MPH; Birmingham, Alabama
By the end of the session, learners will evaluate commonly held assumptions related to vulnerable populations By the end of the session, learners will recognize personal bias related to vulnerable populations
72-QI. Oral Care to Decrease Non-Ventilator Associated Hospital-Acquired Pneumonia
- Susan Kill, MSN, RN, NEA-BC, CNRN; University of Alabama at Birmingham; Birmingham, Alabama
- Cheryl Goodwin, BSN, RN; University of Alabama at Birmingham Medical Center; Birmingham, Alabama
- Rebecca Miltner, PhD, RN, NEA-BC, FAAN; University of Alabama at Birmingham; Birmingham, Alabama
- Cathy Ward, Ph.D, RN, NEA-BC; University of Alabama at Birmingham; Birmingham, Alabama
Describe the most frequent cause of hospital-acquired pneumonia. Identify patients most likely to develop hospital-acquired pneumonia. Describe two components of the nursing intervention that will reduce the incidence of hospital-acquired pneumonia. Discuss the conceptual framework that supports the transition of evidence-based knowledge into sustained nursing practice.
 |
73-R. Faculty Decisional Involvement Scale Development
- Nancy Ballard, PhD, RN, NEA-BC; Kennesaw State University; Kennesaw, Georgia
- Lynn Varagona, PhD, MBA, RN; Kennesaw State University; Kennesaw, Georgia
- Modupe Adewuyi, PhD, MSN/MPH, PHNA-BC, CHES; Kennsaw State University; Kennesaw, Georgia
- Margot "Lisa" Hedenstrom, PhD, RN, MBA, NEA-BC; Kennesaw State University; Kennesaw, Georgia
Identify two elements of the faculty decisional involvement scale. List two areas in which faculty usually participate regarding decisions at the department level.
- DANIELLE SARAIVA TUMA DOS REIS, Profa da Universidade Federal do Pará; Universidade Federal do Pará; Belém, Brazil
- MARA REGINA ROSA RIBEIRO, Profa da Universidade Federal do Mato Grosso; Universidade Federal do Mato Grosso; Cuiabá, Brazil
- Hadelândia Milon de Oliveira, Prof da Universidade Federal do Amazonas; Universidade Federal do Amazonas; Manaus, Brazil
- José Luis Guedes dos Santos, Professor da Universidade Federal de Santa Catarina; Universidade Federal de Santa Catarina; Florianópolis, Brazil
- Gabriela MARCELLINO DE MELO LANZONI, Professor da Universidade Federal de Santa Catarina; Universidade Federal de Santa Catarina, Brazil
To evaluate the perception of nurses about the environment of professional nursing practice generated during the provision of care to patients with Covid-19 residing in the Brazilian Amazon, using the Practice Environment Scale - PES instrument. To measure the care product through the APROCENF instrument, developed to classify the product generated at the end of the nursing work shift in hospitals in the Brazilian Amazon. To correlate the two instruments PES and APROCENF in the pandemic scenario of the Brazilian Amazon.
77-EBP. A Program Evaluation of the Atrium Health Mentoring Program for Women on the Road to Success (MPWRS)
- Patricia Mook, MSN, RN, NEA-BC, CAHIMS, FAONL; Advocate Health; Charlotte, South Carolina
understand how does the Mentoring Program for Women on the Road to Success improved individual leadership self-efficacy? Understand How the MPWRS program supports retention, promotion and goal attainment of Managers and Directors.
- Patricia Patrician, PhD, RN, FAAN; University of Alabama at Birmingham; Birmingham, Alabama
- Aoyjai P. Montgomery, PhD, BSN; University of Alabama at Birmingham; Birmingham, Alabama
- Allyson G. Hall, PhD, MBA, MHS; University of Alabama at Birmingham; Birmingham, Alabama
- Shea Polancich, PhD, RN, FAAN; University of Alabama at Birmingham; Birmingham, Alabama
- Rebecca (Suzie) Miltner, PhD, RN, FAAN; University of Alabama at Birmingham; Alabama, Alabama
Explain the why leaders should be concerned with tracking patient experience data. Discuss differences between patient experience ratings among patients with and without COVID-19 and state possible reasons for these differences.
82-EBP. Nursing is Not Multiple Choice
- Mithun Mahinda, CCRN, CMC; UCLA Health; Santa Monica, California
Increase retention rates of new staff (new hires and new graduates RNs) by conducting a needs assessment of key stakeholders such as nurse managers, preceptors, preceptees. Promote clinical advocacy by providing clinical resources and education that aims to bridge nursing school (Test-based mentality) to the bedside (clinical decision-making mentality). Support class instructors and preceptor development by providing promoting teaching resources that are consistent in delivery and alignment of best practices of the organization.
- Teresa Dodd-Butera, PhD; RN/DABAT; Azusa Pacific University; Azusa, California
- Marissa Brash, DrPH, EdD, MPH, CPH; Azusa Pacific University; Azusa, California
- Nga Nguyen, MPH, MAiL; Arcadia, California
Define emergency preparedness competencies, based on professional and educational standards for professional nursing. Discuss strategies for developing emergency preparedness and training for future and current professional nurses. Identify the role of nursing leaders in advocating for equity in emergency preparedness through workforce development and preparation.
84-EBP. Assessing the Effectiveness of the University of Alabama Birmingham. STEMI Program: A Program Evaluation of Performance Measures and Outcomes for UAB STEMI Patients
- Sherri Wall, MSHA, BSN, RN, CNOR; UAB School of Nursing; Birmingham, Alabama
To evaluate the effectiveness of UAB STEMI program Determine if UAB STEMI Program meets industry standards for treatment of the STEMI patient Analyze data on patient outcomes for mortality rates and perfusion times
Presenters Alphabetical by Last Name/Surname Louisette Abikou, MPH, RN; University of Cincinnati; Cincinnati, Ohio Louisette Abikou is a current PhD student at the University of Cincinnati's College of Nursing, focusing on addressing health and social inequalities related to gender-based discrimination. With her extensive nursing background, Louisette is deeply committed to conducting research that is both culturally and situationally tailored to women's needs. Her overarching aim is to improve the health outcomes of women on both national and global levels. Modupe Adewuyi, PhD, MSN/MPH, PHNA-BC, CHES; Kennsaw State University; Kennesaw, Georgia Dr. Adewuyi is an assistant professor at the WellStar School of Nursing at Kennesaw State University with over 11 years of experience teaching undergraduate and graduate population-based and research-related courses. Her research program centers around vulnerable populations, with a particular focus on dementia. She has served as PI or co-PI on multiple research projects and has secured internal and external funding, most recently from the National League of Nursing. Dr. Adewuyi is a prolific author and co-author of numerous data-based articles, abstracts, and book chapters. Ida Anderson, MSN, RN, NEA-BC, ONC; UCLA Health; Los Angeles, California Ida Anderson, MSN, RN, NEA-BC, ONC is an experienced nursing leader who has served in progressive nursing leadership roles for the past 15 years. She is currently the Director of Adult Critical Care Nursing at Ronald Reagan UCLA Medical Center. In this role, she has quality, safety, and operational responsibilities for five adult critical care nursing units, the Cardiac Observation Unit, and the Critical Care Transport Team which provides both ground and air transport services for neonates, pediatrics, and adults. Ms. Anderson earned her Baccalaureate nursing degree from the University of Colorado and her Masters in Nursing Leadership from Grand Canyon University. Ziyah Anderson, BSKin, (MSHMI expected July 2023); Kennesaw State University; Kennesaw, Georgia Currently in the final semester of the Master’s in healthcare management and Informatics program at Kennesaw State. She serves as an Implementation Project Manager for Meditech. She has healthcare experience including work in human resources and as a CNA as well as a BSKin from Georgia Southern University. She has a passion for supporting healthcare work and was instrumental in developing this analysis in Gen Z. She is part of the Gen Z population and seeks to help leaders improve their knowledge and understanding of this group of nurses ViAnne Antrum, DNP RN MBA NEA-BC CENP FACHE; Cone Health; Greensboro, North Carolina Dr. Vi-Anne Antrum is a seasoned executive with nursing and operations experience spanning over 25 years. She currently serves as the Systemwide Chief Nursing Officer and Senior Vice President for Cone Health, an integrated health system in Greensboro, NC. Dr. Antrum has contributed to the body of nursing knowledge through a variety of publications, presentations, and taskforces. She holds an MBA from University of Phoenix and her DNP in systems-level leadership from Thomas Edison State University. She is board certified in executive nursing leadership by AONL and ANCC and is a Fellow of the American College of Healthcare Executives. Chika Anueyiagu, DNP,RN, FNP, NE-BC; Yale New Haven Health; new haven, Connecticut Dr Anueyiagu is the Director of Surgical Services at Yale New Haven Hospital with oversight of Inpatient surgical units including, surgical intensive care, trauma, intermediate care, bariatric, general surgery, vascular, and minimally invasive surgery units. She has leadership experience spanning over 20 years in several roles across specialties and settings. In these roles, she had the responsibility of alignment and execution of strategic initiatives while ensuring excellent outcomes in nurse sensitive indicators. Chika earned her Doctor of Nursing Practice Degree from Fairfield university in Executive Leadership. She obtained her Nurse Executive Board certification through the American Nurses Credentialing Center. Sandra Anyoha, DNP, MSN , MPH, RN, FNP CNML; Yale New Haven Health; new haven, Connecticut Dr. Anyoha is a Patient Services Manager at YNHCH with the primary responsibility for operations and oversight of two inpatient pediatric units. She is a certified Nurse manager and Leader with extensive experience in both outpatient and inpatient Nursing operations. Sandra belongs to several Nursing organization and is the Founder and a board member of (NANNNA). Sandra has received numerous leadership awards and was a recipient of the “Florence Nightingale “award in the state of Connecticut. Sandra holds a Doctorate in Nursing from the University of Massachusetts and an MSN /MPH from Hunter college in New York. Edwin Aroke, PhD, FAANA, FAAN; University of Alabama at Birmingham; Birmingham, Alabama Dr. Edwin Aroke is an Associate Professor and the Director of the Ph.D. Program at the UAB School of Nursing. His NIH-funded program of research examines the role of epigenomic changes on chronic pain and pain disparities. Dr. Aroke has received numerous prestigious awards, including, Researcher of the Year by the American Association of Nurse Anesthesiology (AANA) Foundation, Didactic Faculty of the Year by the AANA, and Mitchell Max Award for Research Excellence from the NIH. He doubles as a Fellow of the American Association of Nurse Anesthesiology and a Fellow of the American Academy of Nursing. Julia Aucoin, DNS, RN, NPD-BC; UNC Health Rex; Raleigh, North Carolina 44 years nursing experience, 42 years in practice and education implementation. National and international consultant for nursing excellence. Experienced presenter and numerous publications. Lissette Aviles, Lecturer; University of Edinburgh; Edinburgh, United Kingdom Lissette earned her Professional Degree in Nursing (RN) and Bachelor of Science in Nursing (BSN) at Universidad de Concepcion, Chile. She completed her Master of Nursing at Pontificia Universidad Catolica de Chile and Ph.D. Nursing Studies at the University of Edinburgh. She is keenly interested in qualitative methods, grounded theory, the social sciences, nursing theory, and ethical considerations in conducting research and is currently working as a Lecturer in Nursing Studies at the University of Edinburgh. Cindy Bacon, PhD, RN, CNE, NE-BC; University of North Carolina at Greensboro; North Carolina, North Carolina Associate Professor and Program Director, MSN Programs (Interim) at the University of North Carolina at Greensboro School of Nursing. ANS Faculty Advisor K. David Bailey, PhD, MBA, RN, CCRN-K, NEA-BC, FACHE, FAAN; UCLA Health - Santa Monica Medical Center; Santa Monica, California Dr. Bailey is the Chief Nursing Officer at UCLA Health – Santa Monica Medical Center, a Magnet-designated organization. Dr. Bailey is an Adjunct Assistant Professor at the UCLA SON in the DNP Program and an Adjunct Professor at the FPB SON at Case Western. Before joining UCLA Health, Dr. Bailey worked in several southeastern states in leadership roles. Dr. Bailey is the Past-President of the Association for Leadership Science in Nursing, an international organization focused on shaping leadership science, research, and education for academic and practice partners. He is a Board Member for WISE and Healthy Aging, a not-for-profit organization headquartered in Santa Monica, CA, that provides services for older adults in LA and San Bernardino counties. Dr. Bailey is a member of Viven Health’s Clinical Advisory Council, an organization focused on simulated learning to change behaviors. Dr. Bailey holds a Ph.D. and MBA from the University of Phoenix and an MSN and BSN from the Medical University of South Carolina. He is certified in critical care and executive nursing and a Fellow of the American College of Healthcare Executives. In 2022, Dr. Bailey was inducted as a Fellow of the American Academy of Nursing. He has authored or co-authored numerous nursing leadership articles on various topics and is a peer reviewer for four professional journals. Dr. Bailey is enrolled in the Coldiron Senior Nurse Executive Program at the Marian K. Shaughnessy Nurse Leader Academy at the Frances Payne Bolton School of Nursing at Case Western Reserve University. Nancy Ballard, PhD, RN, NEA-BC; Kennesaw State University; Kennesaw, Georgia Following a career in a large healthcare system with varied leadership roles, Dr. Nancy Ballard is an Associate Professor at Kennesaw State University in Kennesaw, GA where she coordinates the Nursing Administration Program. As a Nurse Scientist, her research interest focuses on nursing leadership and the impact of the practice environment on quality and operational outcomes. She has published and presented nationally and internationally on her work in this area. Gilbert Barco, MSN, RN, CCRN; UCLA Health; Los Angeles, California Gilbert Barco, MSN, RN, CCRN is the Assistant Director for the Nursing System Float Team at UCLA Health overseeing the Critical Care Float Team. Gilbert obtained his Bachelor’s degree in Business Administration and went on to pursue a second career in Nursing, obtaining his second Bachelor’s then continuing to his Master’s in Nursing Administration. Gilbert has been a nurse for 11 years, beginning his nursing career in ICU where he developed strong leadership skills that have helped him excel in his current role. His leadership and guidance have been instrumental in achieving positive outcomes. Janene Batten, EdD, MLS,; Yale University; New Haven, Connecticut Dr. Batten is the Senior Nursing Research & Education Librarian in the Cushing/Whitney Medical Library, Yale University. Her expertise is connecting people and ideas to ensure the inclusion of diverse perspectives. She consults and collaborates with clinical nurses on pressing clinical issues and assists world-class clinical nurse researchers with their research. She also helps nursing faculty and students, supporting best-in-class scientific research and teaching in various nursing graduate programs. Janene earned her EdD in Organizational Change and Leadership from the Rossier School of Education, University of Southern California. She is a Board Member of the Connecticut Center for Nursing Workforce. Pamela Baxter, RN,PhD; McMaster University; Hamilton, Canada Dr. Pamela Baxter has a program of research focusing on examining and developing healthcare leadership to meet the growing demands of healthcare systems provincially, nationally, and internationally. Her research focuses primarily on issues/challenges faced by those providing leadership in long-term, palliative, and end of life care settings. To achieve this goal, she has engaged in a variety of research projects funded by organizations such as the Canadian Institute of Health Research, the Ontario Ministry of Health and Long-term Care, the Canadian Nurses Foundation, and the Canadian Health Services Research Foundation. Angie Blevins, RP, OSBA, CPHRM; Wexner Medical Center at The Ohio State University; Columbus, Ohio Angie Blevins, RP, OSBA, CPHRM has over 33 years of paralegal experience. She has held the titles of licensed practice nurse, paralegal, risk analyst, and senior litigation risk analyst. After earning her certificate in Practical Nursing from Temple Junior College, she went on to earn A.A.S. in Paralegal Studies from Central Texas College. She is a Registered Paralegal through the National Federation of Paralegal Associations, an Ohio State Bar Association Certified Paralegal, and an American Hospital Association Certified Professional in Health Care Risk Management. Curry Bordelon, DNP, MBA, NNP-BC, CPNP-AC, CNE; University of Alabama at Birmingham; Birmingham, Alabama Curry Bordelon is an Associate Professor and Assistant Dean for Graduate Clinical Education-DNP Program for the University of Alabama at Birmingham School of Nursing. Dr. Bordelon has extensive leadership experience as a nurse practitioner manager, Executive Committee for the Academy of Neonatal Nurses, Vice President for the American Associate for Men in Nursing, and President for the UAB Nu at-Large Chapter of Sigma. Curry participates in the Curricula Leadership Committee for NONPF and led a curricula taskforce for AACN to develop curricula toolkits for faculty. Curry has several publications and presentations focusing on teaching innovations, neonatal care, curricula, and leadership. Marissa Brash, DrPH, EdD, MPH, CPH; Azusa Pacific University; Azusa, California Marissa Brash, DrPH, MPH, CPH, is the chair of the Department of Public Health. She also serves as an Associate Professor in the School of Nursing. Throughout the last decade, she has been working in higher education and has been responsible for developing new academic programs at multiple Southern California institutions. Brash is nationally certified in public health and has a strong background in biostatistics and epidemiology. Her research interests include epigenetic-based autoimmune public health prevention efforts through lifestyle interventions, and neuroeducation topics related to academic stress and anxiety in the STEM subjects. Sylvia Britt, PhD, RN; Birmingham, Alabama Dr Sylvia Britt is a retired Assistant Professor of Nursing. During her 25+ year career she was program director for the MSN Accelerated Pathway and taught across RN to BSN and BSN programs. She received Bachelor of Nursing Science at the Medical College of Georgia, and Mater of Nursing Science and PhD at University of Alabama at Birmingham. She serves as an academic mentor to former students and performs community nursing as a volunteer in her community. Susan Campis, MSN, RN, NE-BC, NBC-HWC; uLeadership; Atlanta, Georgia Susan Campis is a nurse executive, author, and Certified Health and Wellness Coach. Susan began her nursing career in the ICU where she was a staff nurse for 15 years before moving into a formal leadership role. Over the years, she served as Nurse Manager, Director, and Executive Director. Susan is a nurse leader whose passion for coaching and mentoring produce engaged nursing teams throughout her career. Susan cares deeply for the well-being of health care professionals and, as a Certified Health and Wellness Coach, her goal is to work with others to help them reach their full potential. Julia Gonçalves Escossia Campos, Nurse; Universidade Federal do Rio de Janeiro, Brazil Nurse from the Federal University of Rio de Janeiro. Master student in nursing at the Anna Nery Nursing School/UFRJ. Esther Chipps, PhD, RN, NEA-BC, FAONL; The Ohio State University; Charlotte, North Carolina Dr. Esther Chipps holds a dual appointment at The Ohio State University as the Nurse Scientist at The OSU Wexner Medical Center and as a Professor of Clinical Nursing at The Ohio State University College of Nursing. She has conducted over 40 studies and has published over 55 manuscripts impacting the practice areas of critical care, medical-surgical, rehabilitation, transplant, women/infants nursing, and nursing leadership. She is a Fellow in the American Organization for Nursing Leadership Jeannie Corey, DNP,RN,NEA-BC; James Madison University; Harrisonburg, Virginia Jeannie Corey DNP, RN, NEA-BC, is a Professor of Nursing in the Doctor of Nursing Practice program at James Madison University (JMU). Prior to joining JMU, she was faculty at Jefferson College of Health Sciences and Virginia Tech Carilion School of Medicine. She received her DNP from Case Western Reserve University, MSN from the University of Virginia, BSN in Nursing from Radford University, and an AD from Virginia Western Community College. She has many years of executive, leadership, clinical, and higher education experience. Research interests are DNP project practices, health policy, leadership moral distress, and interprofessional practice and education. Nancy C Crider, DrPH, MS, RN, NEA-BC; Cizik School of Nursing at University of Texas Health Science Center – Houston; Houston, Texas Dr. Nancy Crider is an accomplished nursing leader and educator. She has held numerous executive leadership positions in both large tertiary academic medical centers and smaller community hospitals. She is certified by ANCC (NEA-BC) and is an active member of numerous professional organizations. Crider currently, teaches leadership, business, and health policy in the Department of Graduate Studies DNP program at Cizik School of Nursing at the University of Texas Health Science Center - Houston. Jade Cruz is a Nursing Professional Development Specialist who oversees student placement, preceptor development, and ECG programs. Jade was the Simulation Education Specialist at Emory University Hodgson Woodruff School of Nursing and responsible for developing the Simulation Program in the Bachelor's and Master's Degree Programs. Prior Nursing Education experience includes stints at the Mayo Clinic in Phoenix as the Simulation Education Specialist, and Nursing Education Specialist, where she was responsible for simulation education and system wide training. Jade is currently a mentor of Professional Governance Councils and has been instrumental in the development of Nursing EDI council at UCLA Health. Martha A. Dawson, DNP, RN, FAAN, FACHE is an Associate Professor at UAB School of Nursing. Dr. Dawson is the 13th president of the National Black Nurses’ Association. She earned her bachelor’s and master’s degree from the University of Alabama at Birmingham School of Nursing. In 2010, she earned her Doctor of Nursing Practice from Case Western Reserve University Frances Payne Bolton SON. Dr. Dawson completed her hospital administration residency at Gaston Memorial Hospital, Gastonia. NC. Her practice, leadership and clinical research focuses are in the domains of administrative systematology, career progression, organizational injustices and barriers, and equality in nursing. She has served in senior level hospital positions. She is a co-convenor of the 2020 National Black Coalition Against COVID reaching over five million during the pandemic and a co-lead of the 2020 National Commission Addressing Racism in Nursing which is ground breaking work to improve healing within the nursing profession. Dr. Dawson serves on the Advisory Board for Direct Relief Health Equity Fund that is allowing her to address social justice and SDOHs through the act of generous donors has awarded 170 grants providing 42.2 million to address health inequities. She is a Scholar in UAB Sparkman Global Health Center, American College of Healthcare Executives Fellow, Robert Wood Johnson Nurse Executive Fellow alumina, and a Johnson & Johnson Wharton Nurse Administrative Fellow, alumina. In 2019, Dr. Dawson was inducted into the Alabama Nurses Hall of Fame, 2021 honored as a UABSON visionary leader and 2022, president of the year by the American Nurses Associations. She has received the UAB President’s Excellence in Teaching Award, UAB Dean’s Mentorship Award, and the American Organization of Nurse Leaders Prism Award. In 2022, she became a Fellow in the American Academy of Nursing and appointed as an associate scientist in the Social Science and Justice Research Center and in 2023 she joined as a Center Scholar in the UAB Center for the Study of Community Health, one of 26 Prevention Research Centers designated by the CDC nationally as an interdisciplinary research center. She has publications in books, journals, newsletters, op-eds and podcasts. The University of Louisville Hospital, where she served as CNO and vice president was first to provide drive through flu shots in the US; the model that the CDC has used during COVID-19. She was a contributing author in the Drive-Thru Flu Shots: A model for mass immunization. She is dynamic speaker and workshop leader. In 2006, the Martha A. Dawson Genesis Scholarship was established with the National Black Nurses Association. Stephan Davis, DNP, MHSA, NEA-BC, CENP, CDE, CNE, CPHQ, FACHE, FNAP, FHFMA, FAAN; Virginia Commonwealth University; Richmond, Virginia Stephan serves as the Associate Dean for Inclusive Excellence and Belonging for both VCU College of Health Professions and the VCU School of Nursing. He is also the inaugural executive director of inclusive leadership education for the VCU Department of Health Administration. Dr. Davis is a fellow and national faculty member for the American College of Healthcare Executives (ACHE). He previously chaired the ACHE LGBTQ Healthcare Leaders Community and has served as an ACHE Regent-at-Large, a role created to foster diversity in the governance of ACHE. He has also been appointed by the American Academy of Nursing's Board of Directors to the Equity, Diversity, and Inclusivity committee for a two-year term. He is a 2023 recipient of the Association of University Programs in Health Administration’s teaching excellence award for his contributions related to DEI. In addition to fellowship with ACHE, Dr. Davis is a distinguished scholar and fellow of the National Academies of Practice, a fellow of the Healthcare Financial Management Association, and a fellow of the American Academy of Nursing. He holds numerous board certifications including credentials in executive nursing leadership, healthcare quality, strengths-based coaching, and executive diversity leadership. He holds a Doctor of Nursing Practice degree in healthcare leadership and policy from Yale, a post-graduate certificate in evidence-based teaching in the health professions from Johns Hopkins, a master’s degree in health systems administration from Georgetown, and a bachelor’s degree in nursing from University of Maryland. Suja Davis, PhD, RN; University of North Carolina at Chapell Hill; Chapel Hill, North Carolina Dr. Davis is an experienced nurse educator with teaching experience between two continents. Her primary teaching responsibility is with the UG department, but she teaches across the masters and PhD divisions. She obtained a diversity certificate and has incorporated the principles she learned into her classroom clinical,and her global health teaching . Her research work is focused on nursing education and gastrointestinal nursing.She has presented at local, regional, statewide, national and international conferences and has mentored numerous students in the past. Kathleen Diatta, Ph.D., RN, NE-BC is the Nurse Practice Specialist for complex medicine and Acute Respiratory Care Unit at Emory University Hospital. She has 37 years of critical care and perioperative nursing experience. Kathleen spearheaded the development of the nurse residency program at Mt. Sinai Hospital in New York City. She used her experiential knowledge to co-develop the nurse residency program for the perioperative area at Emory Healthcare. Kathleen is a member of the American Nurses Association, Georgia Nurses Association, American Association of Critical-Care Nurses, Sigma Theta Tau, American Organization for Nurse Leaders, and American Society of PeriAnesthesia Nurses. Tracey Dick; Birmingham, Alabama Tracey Dick, PhD, RN, CNE, COI is an Assistant Professor at the University of Alabama at Birmingham. She is a VA Quality Scholars Fellow and an Associate Scientist in the Center for Clinical and Translational Science (CCTS). Tracey K. Dick, PhD, RN, CNE, COI; UAB School of Nursing; Birmingham, Alabama Tracey Dick, PhD, RN, CNE, COI has been a registered nurse in the state of Alabama for 34 years. Her research focuses on nursing workforce supply, demand, and nursing’s impact on health care quality and safety. Her clinical background spans multiple practice areas including critical care, specialty (GI), physical rehabilitation, and primary care. Dr. Dick has served as a faculty member for 14 years and is currently an Assistant Professor at UAB School of Nursing. She is also currently appointed as a VA Quality Scholar Fellow with the Birmingham VA Health Care System. Maja Djukic, PhD, RN, FAAN; UTHCS Cizik School of Nursing; Houston, Texas Maja Djukic, PhD, RN, FAAN, is a nationally recognized nurse scholar with a program of research focused on nursing workforce determinants of healthcare quality, including expertise in identifying nursing education gaps and developing technology-mediated solutions. Dr. Djukic has pioneered national research of new graduate nurses to identify key gaps in quality and safety competencies essential for high-value patient care. To close the identified competency gaps, Dr. Djukic led inter- professional research teams and academic-practice partnerships to design novel teamwork, quality improvement, and population health management workforce interventions using in-person and virtual simulations. Teresa Dodd-Butera, PhD; RN/DABAT; Azusa Pacific University; Azusa, California Teresa Dodd-Butera, PhD, RN/DABAT, is a registered nurse and a board-certified toxicologist (Diplomate, American Board of Applied Toxicology/ DABAT). She is a Professor of Public Health and Doctoral programs, and serves as the Associate Dean for Research at Azusa Pacific University School of Nursing. Her research focus includes acute and chronic exposures, especially to the maternal-fetal environment. She is also interested in multiple factors that affect global and national maternal-child and family health issues, including families with special needs. She has published on emergency preparedness and select priorities of the Sendai Framework for Disaster Risk Reduction (2015-2030). Sharon Doggett, MSN, RN, NEA-BC; UCLA Health; Los Angeles, California Nursing System Float Team Manager with 20 years of nursing experience including 10 years in management. Focused on providing excellent compassionate care to all patients. Has presented at multiple pediatric and leadership conferences to improve patient care, staffing processes and outcomes. Focused on implementing equitable and inclusive practices in the nursing profession to ensure equitable resources available to provide excellent patient care and improve nursing processes. Mary Dolansky, PhD, RN; Case Western Reserve University; cleveland, Ohio Dr. Dolansky is the Sarah Cole Hirsh Associate Professor of Nursing at the Frances Payne Bolton School of Nursing, Associate Professor School of Medicine Case Western Reserve University (CWRU), Senior Faculty in the Veterans Administration Quality Scholars (VAQS) program at the VA Northeast Ohio Healthcare System, and Nurse Advisor for the national VAQS program. Dr. Dolansky is now the director of the Hirsh Institute which integrates implementation science and practice to improve the quality and safety of healthcare. Her current research includes the implementation of the Institute for Healthcare Improvement evidence-based Age-Friendly Health Systems into the 1,100 MinuteClinics across the country. Yvonne Eaves, PhD, RN; University of North Carolina Greensboro (UNCG); Greensboro, North Carolina Yvonne D. Eaves, Ph.D., RN, is the Associate Dean for Academic Programs and Professor of Nursing at the University of North Carolina Greensboro (UNCG). Previously, she was an Associate Professor and Director of the Wellstar School of Nursing at Kennesaw State University. Early in her career, Dr. Eaves held faculty positions at the University of Alabama at Birmingham and UNC Chapel Hill. Dr. Eaves holds a Ph.D. in nursing from the University of Michigan. Her research has examined caregiving, stroke, caregiving transitions, and long-term care decision-making in rural African American families. Alacoque Lorenzin Erdmann, Full Professor; Universidade Federal de Santa Catarina; Florianópolis, Brazil Ph.D. in Nursing from the Federal University of Santa Catarina - UFSC and earned his Professional Degree in Nursing (RN) at the same University (1975). She is a Full Professor in the Nursing Department and Permanent Professor in the Postgraduate Program in Nursing. She has supervised Master's and Doctoral degrees at UFSC since 1990. Pariya Fazeli, PhD; University of Alabama at Birmingham; Birmingham, Alabama Dr. Pariya Fazeli is an experimental psychologist with academic training in lifespan development, cognitive aging, and gerontology. Her primary research interests include cognitive aging among older adults with HIV, with a focus on predictors of successful cognitive aging as well as rehabilitation strategies to promote successful cognitive aging in this population. Her work is currently funded by the National Institute on Aging. Haley Fenn, MS; Birmingham, Alabama Haley Fenn is the program manager for Nurse Family Partnership of Central Alabama. Carlos Leonardo Figueiredo Cunha, Prof da Universidade Federal do Maranhão; Universidade Federal do Maranhão; São Luis, Brazil Graduação em Enfermagem pela Universidade Estadual do Maranhão (UEMA). Especializações em Programação e Políticas de Saúde. Mestrado em Saúde Materno Infantil pela Universidade Federal do Maranhão (UFMA). Doutorado em Saúde Coletiva pelo Instituto de Estudos em Saúde Coletiva- (IESC/ UFRJ). Experiência na área de Enfermagem em Saúde Coletiva, com ênfase em Políticas e Gestão em Saúde e Atenção Primária. Professor Adjunto do Departamento de Saúde Pública da Universidade Federal do Maranhão (UFMA). John FitzGerald, MA in Psychology, Organizational Behavior concentration; Case Western Reserve University; Cleveland, Ohio Jack FitzGerald, MA, is the Manager of Marian K. Shaughnessy Nurse Leadership Academy programs at the Frances Payne Bolton School of Nursing at Case Western Reserve University in Cleveland, OH. He is co-founder of the Warren Bennis Leadership Institute at the University of Cincinnati where he earned a Master of Psychology degree with a concentration in organizational behavior. Joyce Fitzpatrick, PhD, MBA, RN, FAAN, FNAP; Case Western Reserve University; Ohio, Ohio Dr. Joyce Fitzpatrick is the Director of the Marian K. Shaughnessy Nurse Leadership Academy and Elizabeth Brooks Ford Professor of Nursing at Case Western Reserve University's Frances Payne Bolton School of Nursing in Cleveland, Ohio. She has extensive experience in nursing education, research, and leading national large-scale projects. Dr. Fitzpatrick has specific expertise in nursing leadership development using Narrative Nursing (NN) to address moral injury and has led a significant project in this area. She is also a member of a research team studying mindfulness interventions, showcasing her diverse skills in leadership development and nursing research. Lozay Foots III, DNP, MS, FACHE; San Antonio, Texas Colonel (R) Lozay Foots III previously served as the Deputy Chief of the Army Nurse Corps, he also served as the CNO/Director for Nursing for Walter Reed National Military Medical Center. Prior he served as the Chief, Army Nurse Corps Branch at Human Resources Command, Fort Knox, Kentucky. Past assignments: Deputy Commander of Inpatient Services, Carl R. Darnall Army Medical Center, Fort Hood Texas. Most notably as the Assistant Deputy for Medical Affairs for the Assistant Secretary of the Army for Manpower and Reserve Affairs (ASA M&RA) at the Pentagon. His focus and passion is on developing and growing future nurse leaders. Karen Fowler, Ph.D., RN, CENP; University of Texas at El Paso; El Paso, Texas Dr. Karen Fowler is an Associate Dean of Graduate Studies at the University of Texas at El Paso. Before this, she was a Chief Nursing Officer at an acute care facility. She has conducted leadership research and has several publications related to leadership in nursing. Joana de Oliveira Pantoja Freire, Registered Nurse; Universidade Federal do Rio de Janeiro; Rio de Janeiro, Brazil Master's degree from the Anna Nery School of Nursing Postgraduate program - UFRJ. Multiprofessional residency in nosocomial infection control at the Clementino Fraga Filho University Hospital - HUCFF/UFRJ. MBA in Health Management and Infection Control by FAMESP - SP. Graduation from the Anna Nery Nursing School of the Federal University of Rio de Janeiro - EEAN/UFRJ. Nurse at the Clementino Fraga Filho University Hospital - UFRJ, where she develops infection control and patient safety activities. Nurse at the Hospital Infection Control Service at the Evandro Chagas National Institute of Infectology of the Oswaldo Cruz Foundation (SCIH-INI-Fiocruz). Etiane de Oliveira Freitas, Assistant Professor; Universidade Federal de Santa Maria; Santa Maria, Brazil Nurse. Bachelor's, Master's, and Doctorate in Nursing from the Federal University of Santa Maria (UFSM). Professor at the Department of Nursing at the Federal University of Santa Maria (UFSM). Permanent Professor of the Graduate Program in Nursing. Member of the Research Group: Work, Health, Education and Nursing / UFSM. Associate Editor of the UFSM Journal of Nursing (REUFSM). She has experience in Nursing, working mainly on: nursing care for adults; intensive care nursing (adult, cardiac and neonatal); nursing education; work process in health and nursing; and patient safety. She has an affinity for quantitative research methods and mixed methods studies. Adam Fronczek, DNP, MBA, RN, NEA-BC, ANP-BC; UCLA Health; Los Angeles, California Adam Fronczek, DNP, RN, MBA, ANP-BC is the director of the Nursing System Float Team for UCLA Health. Adam has 15 years of nursing experience with 5 years in leadership. Adam received his bachelor’s and Master of Science in nursing from the University of South Florida and his doctorate in nursing practice from Chamberlain College of Nursing, Chicago. He completed his Master of Business Administration in 2021. Suzanne Gagnon, PhD; University of Manitoba; Winnipeg, Canada Dr. Suzanne Gagnon, Canada Life Chair in Leadership Education, and Associate Dean, Professional Graduate Programs and Executive Education at the Asper School. In addition to her associate deanship, Dr. Gagnon is the inaugural Director of the James W. Burns Leadership Institute, designing and directing new programming across disciplines including the flagship President’s Student Leadership Program. Dr. Gagnon conducts seminal research that focuses on identity, inclusion, and leadership development in international firms; leadership and innovation in diverse contexts; and gender equity, representation, and strategic change in private and public sector organizations. Sandra Galura, PhD, RN; University of Central Florida; Orlando, Florida Sandra Galura, PhD, RN, is an Assistant Professor at the University of Central Florida College of Nursing where she serves as the Director of the Master’s in Nursing Leadership and Management program. Dr. Galura’s program of research focuses on frontline nurse managers and issues influencing their practice environment. She has led several funded research studies, one of which informed the development of this EBP leadership resource. Dr. Galura currently serves on the ALSN membership committee and was awarded the 2022 ALSN Early Careerist Award. Marlon Garza Saria, Ph.D., RN, AOCNS, NEA-BC, NPD-BC, FAAN; Providence St. Johns; Santa Monica, California Marlon Garzo Saria is the Nurse Scientist and Director of Advanced Nursing Practice at Providence Saint John’s Health in Santa Monica, California. He is also a Lieutenant Colonel in the U.S. Air Force Reserve and is currently assigned to the 452d Aeromedical Staging Squadron at March Air Reserve Base in California. Dr. Saria is the President-Elect (2022-2024) of the Philippine Nurses Association of America. Dr. Saria earned his bachelor’s degree in nursing from the University of the Philippines, a Master of Science in Nursing, and a Ph.D. from the University of California Los Angeles. He received a Master’s in Military Operational Art and Science from the Air University, US Air Force. He is board certified as an Oncology Nurse, Oncology Clinical Nurse Specialist, Advanced Nurse Executive, and Nursing Professional Development Specialist. He is a Coldiron Senior Nurse Executive Fellow at Case Western Reserve University’s Marian K. Shaughnessy Nurse Leadership Academy at the Frances Payne Bolton School of Nursing. Dr. Saria is a Fellow of the American Academy of Nursing. Dr. Saria has held educational, research, and leadership roles in various oncology settings. He was appointed Visiting Researcher at Chiba University School of Nursing in Japan. He is a lecturer at the University of the Philippines Open University. He is one of the co-investigators and founding members of the Brain Cancer Quality of Life Collaborative and Los Angeles Cancer Caregiver Consortium. He is an associate editor of the Core Curriculum for Oncology Nursing and has published multiple papers and book chapters. Eskedar Gizaw, MSN, RN, NP; UCLA Health; Los Angeles, California Eskedar Gizaw is a hospitalist nurse practitioner at Santa Monica UCLA. Eskedar received her undergraduate degree from University of Kansas and her Master's Degree at University of California Los Angeles. Eskedar has worked as a bedside nurse in the step-down unit at UCLA serving as charge nurse prior to becoming a nurse practitioner. She has been part of the hospitalist group for over a decade and been involved with creating discharge nurse practitioner. She is currently serving as Unity in Diversity co-chair, a member of emergency response committee and involved in several process improvement initiatives. Ph.D. student in Nursing at the Anna Nery Nursing School/UFRJ. Nurse from Universidade Federal Fluminense (2001), Specialization in Prevention and Control of Hospital Infections from Universidade Gama Filho, and Specialization in Quality and Patient Safety from ENSP-FIOCRUZ. She is currently a nurse at the Lourenço Jorge Hospital of the Health Department of the Municipality of Rio de Janeiro and the Clementino Fraga Filho University Hospital of the Federal University of Rio de Janeiro (HUCFF/UFRJ). Cheryl Goodwin, BSN, RN; University of Alabama at Birmingham Medical Center; Birmingham, Alabama Cheryl Goodwin, RN, BSN works at the UAB Department of Infection Prevention. She is a 1996 graduate of the UAB School of Nursing and has worked in various roles at UAB Hospital/UAB Health Services Foundation since 1997. Changing mindsets through staff education is Cheryl's wheelhouse and how she intends on achieving the goal of HAP prevention. Martha Grubaugh, PhD, RN, NE-BC; UCHealth; Aurora, Colorado Dr. Grubaugh is a Research Nurse Scientist at UCHealth in Colorado and an Assistant Professor at the University of Colorado College of Nursing. She has experience as a pediatric critical care clinician and has spent two decades leading the nursing profession in a variety of managerial and executive positions. Her research has been dedicated to improving and cultivating supportive practice environments for all levels of the healthcare system, with specific attention to the nurse manager. She also has experience researching transition to practice outcomes and has presented on those nationally and internationally. José Luís Guedes dos Santos, PhD, RN; Universidade Federal de Santa Catarina; Florianópolis, Brazil Assistant Professor at Nursing Department, Deputy Coordinator and Director for International Initiatives at Nursing Graduate Program at Universidade Federal de Santa Catarina Brett Hagenbuch, MHA, BSN, RN, NE-BC; The James Cancer Hospital at The Ohio State University; Columbus, Ohio Brett Hagenbuch, MHA, BSN, RN, NE-BC has 9 years of nursing experience. He has held the titles of Staff Nurse and Nurse Manager in several areas of inpatient nursing including med/surg, progressive/intermediate care, and critical care. He completed his BSN at Capital University and MHA at The Ohio State University. He holds a certification as a board-certified nurse executive. His current role is the Nurse Manager for the Neuro Critical Care and Surgical ICU at the James Comprehensive Cancer Center at The Ohio State University Wexner Medical Center. Gayle Halas, PhD; University of Manitoba; Winnipeg, Canada Dr. Gayle Halas is the inaugural Rady Chair in Interprofessional Collaborative Practice, focused on team-based primary health care, and the communication and interactions that enable collaborative practice, particularly for addressing complex needs and care. She builds upon collaborative relationships between educational and practice systems and has been actively involved in developing innovative student-infused learning and practice, research capacity building, data resourcing relevant to the broader health workforce and examining leadership strategies and capacity for fostering teamwork within the health care system. Allyson G. Hall, PhD, MBA, MHS; University of Alabama at Birmingham; Birmingham, Alabama Dr. Hall is a Professor in the Department of Health Services Administration at the University of Alabama at Birmingham. She also serves as Co-director for the University’s Center for Outcomes Effectiveness Research and Education. Dr. Hall’s research focuses on improving access and quality of care among vulnerable patients. Debra Hampton, PhD, MSN, RN, NEA-BC, CENP, FACHE, FAONL; UK College of Nursing; Lexington, Ky, Kentucky Debra Hampton received her MSN and PhD from the University of Cincinnati and has served as a middle manager, chief nursing officer, and CEO. Dr. Hampton is currently the Assistant Dean of the MSN and DNP Programs, the Coordinator of Graduate Leadership programs, and an Associate Professor at the University of KY College of Nursing. Dr. Hampton has also worked FT at Loyola University New Orleans and PT at Franciscan Missionaries of Our Lady University. Dr. Hampton has Advanced, Nurse Executive certification through ANCC and AONL and is a fellow of the American College of Healthcare Executives and AONL. Annette Harrilson, RN, MSN, DNP; Piedmont Fayette Hospital; Fayetteville, Georgia Successful Hospital / Nurse Executive for fifteen (15) plus years focuses on delivering compassionate patient/family-centered care by achieving positive, safe quality outcomes. A transformational leader focuses on investing in the professional development of employees and building a respectful workplace, which fosters functional teams within and across disciplines Dr. Karen Heaton is a Professor at UAB School of Nursing. Her research focuses on the impact of sleep, access to care, and physical health on mental health, cognitive performance, and safety among workers. She served as PhD Program Director from 2014 – 2021 and led the implementation, evaluation, and revisions of the curriculum. Dr. Heaton also serves as faculty for the Deep South Center for Occupational Safety and Health, a NIOSH – funded Education and Research Center. She is a Fellow of the American Association of Occupational Health Nurses (FAAOHN) and a Fellow in the American Academy of Nursing (FAAN). Margot Hedenstrom, PhD, RN, MBA, MSN, NEA-BC; Kennesaw State University; Kennesaw, Georgia Dr.Hedenstrom is an Assistant Professor of Nursing at Kennesaw State University. She has over 30 years of nursing leadership experience in hospital and healthcare systems including roles as a Chief Nursing Officer. She has published and presented on the topic of nursing leadership with a focus on mentoring and supporting the professional development of nurses and nurse leaders. She serves as a Magnet and Pathway to Excellence reviewer for the ANCC. She has been a member of ALSN for three years. Cori Heier, MSN, RN, CNE, CHSE, CNRN; South Dakota State University; Sioux Falls, South Dakota Cori Heier, MSN, RN, CNE, CHSE, CNRN began her nursing career in 2013 after graduating from South Dakota State University. She began teaching at South Dakota State University in 2018 after completing her masters degree at American Sentinel University and has clinical nursing experience in the fields of neuroscience, emergency department, urology and operating room. In 2018, she became a Certified Neuroscience Registered Nurse, in 2021 she became a Certified Nurse Educator, and in 2023 she became a Certified Healthcare Simulation Educator. Cori is pursuing a PhD in nursing and is interested in research related to academic leadership. Teresa Barry Hultquist, PhD, MSN, RN, NE-BC, PHCNS-BC; University of Nebraska Medical Center College of Nursing; Omaha, Nebraska Dr. Barry Hultquist is Professor and Director of Evaluation at the University of Nebraska Medical Center, College of Nursing. She holds ANCC Certifications as Nurse Executive and Clinical Nurse Specialist, Public/Community Health Nursing. Dr. Barry Hultquist teaches at the graduate level in the Nurse Executive/Leader track and DNP program. She has been involved in over 20 funded programs/projects and has published articles related to health status, health services use, population health, quality improvement, and interprofessional education. She has served in leadership roles in several professional organizations, including ALSN and Nebraska Organization of Nurse Leaders District One Finance Committees. Georgia Jackson, DNP, MPH, RN, NE-BC; Emory University Hospital; Atlanta, Georgia Georgia Jackson is the Director Nursing Workforce Development and Patient- & Family-Centered Care and was the co-Principal Investigator of this research study. Stephanie Jackson, DNP, MSN, RN, AOCNS, BMTCN; UCLA; Los Angeles, California Stephanie Jackson is a unit director for the hematology/stem cell transplantation unit at Ronald Reagan Ucla Medical Center. She was formerly a clinical nurse specialist for the inpatient/outpatient hematology/transplantation/cellular therapy program at Ucla as well. Stephanie has served as the president of the Greater Los Angeles Chapter of Oncology Nursing Society. Jin Jun, PhD, RN; Ohio State University; Columbus, Ohio Jin Jun, PhD, RN, is a tenure-track Assistant Professor at The Ohio State University College of Nursing’s (OSUCON) Center for Healthy Aging, Self-Management and Complex Care, Columbus, OH. Dr. Jun’s program of research focuses on empowering, validating, and advocating for workers by optimizing their total health and well-being. Josephine Kamera, Ed.D., RN; Middle Georgia State University; Macon, Georgia Dr. Josephine Kamera is an Associate professor of nursing at Middle Georgia State University, Georgia. Dr. Kamera is the RN-BSN program coordinator. She teaches in the RN-BSN program and other nursing courses. In addition, Dr. Kamera serves as a Subject Matter Expert of Community Health on the Curriculum Leadership Committee of the University System of Georgia eMajor Collaborative Program of Study. Roberta Kaplow, Ph.D., APRN-CCNS, AOCNS, CCRN, FAAN; Emory University Hospital; Brookhaven, Georgia Roberta Kaplow is the Clinical Nurse Specialist for Nursing Research and Evidence-Based Practice at Emory University Hospital in Atlanta, GA. She was the Principal Investigator of this research study. Zhichun Ke, MS; UTHCS Cizik School of Nursing; Houston, Texas Ms. Ke is a doctoral student in the School of Public Health and a graduate research assistant at Cizik School of Nursing. Kay Kennedy, DNP, RN, NEA-BC, CPHQ; uLeadership; Atlanta, Georgia Dr. Kay Kennedy is an author, nurse executive, nurse educator, and entrepreneur. By combining a love for nurses, patients, and quality improvement, she has led large nursing teams to create healthy work environments, satisfied patients, and consistent, high-quality care.She has held multiple leadership roles from the bedside to Chief Nursing Officer. She currently serves on the faculty at Emory University’s Nell Hodgson Woodruff School of Nursing in Atlanta, GA and is adjunct faculty at Massachusetts General Hospital Institute of Health Professions in Boston, MA. Susan Kill, MSN, RN, NEA-BC, CNRN; University of Alabama at Birmingham; Birmingham, Alabama Susan Rieger Kill, MSN, RN, NEA-BC, CNRN earned her BSN from Georgetown University in Washington, D.C., and her MSN from the University of Alabama at Birmingham. Susan is currently a doctoral student in the Executive DNP program at UAB. Areas of expertise include operations, financial management, and strategic planning in hospital operations. Throughout her career, Susan has focused on nursing leadership development and education. She has a passion for coaching and mentoring emerging and early-career nursing leaders. Susan’s ultimate goal is to assure the critical impact of professional nursing on the evolving state of healthcare through scholarship, advocacy, and leadership. Minjin Kim, PhD, RN; University of Cincinnati; Cincinnati, Ohio Dr. Minjin Kim, an Assistant Professor at the University of Cincinnati, focuses on promoting health equity by reducing disparities and improving health outcomes for underserved populations. Her human-centered interventions use storytelling and digital health technologies like AI Chatbots to enhance health communication and accessibility. Dr. Kim prioritizes the human aspect of healthcare to create equitable access to resources. She has received an NIH/NINR K23 grant for a culturally appropriate storytelling intervention using AI chatbot technology for HPV vaccination motivation and an ALSN Foundation Pilot Award to study mini-mindfulness and narrative nursing interventions for nurse leaders' resilience and well-being. Candace Knight, PhD, RN, FAAN; University of Alabama at Birmingham School of Nursing; Birmingham, Alabama Dr. Knight is an Associate Professor at the University of Alabama at Birmingham School of Nursing, where she is the director of the Nurse Family Partnership of Central Alabama and teaches maternal child health nursing. The outcomes generated by the Nurse Family Partnership of Central Alabama team under Dr. Knight’s direction have positively impacted the mental and physical health of these families, improving the preterm birth, breastfeeding, and employment rates of these clients to a rate better than the state and county levels even among statistically disadvantaged women while providing a robust clinical experience for interdisciplinary students. Kimberly Knotts, MSN, RN, NEA-BC; Wellstar Paulding Medical Center; Hiram, Georgia Professional Practice Director at Wellstar Paulding. She received her BSN from the University of Vermont, her MSN from Emory University, and holds certification as a Nurse Executive Advanced. Her nursing background is in orthopedics, critical care, cardiology, and nursing administration. She facilitates Shared Leadership Councils and coordinates the recently designated hospital’s Magnet Recognition Program. She serves on Academic Advisory Councils and coordinates students’ placements. She is a member of Sigma Mu Phi-and AACN where she served as the past President for the local chapter. Research and presentations include poster and podium presentations on various leadership and clinical topics. Mônica Köpsel Fusari, MSc, RN; Universidade Federal de Santa Catarina; Florianópolis, Brazil Registered Nurse and PhD student at Universidade Federal de Santa Catarina Sarah Lackey, DNP RN CMC; Cone Health; Greensboro, North Carolina Dr. Sarah Lackey has broad experience in clinical, staff development, and quality settings; she has published numerous peer reviewed articles; served as an advocate for nursing on various boards and governing bodies; and works with leaders to evaluate and implement solutions. Her 40+ year career in nursing prepares her adequately for the task of deciphering the complex issue of nurse retention. Sarah obtained her Doctor of Nursing Practice degree in systems leadership at the University of Alabama; her Master’s degree at the University of Alabama at Birmingham; her BSN from Northern Illinois University. She is a certified professional coach. Anila Ladak, DNP, RN, CNS, GNP-BC; UCLA; Los Angeles, California Anila Ladak is a Geriatric Clinical Nurse Specialist for UCLA Santa Monica hospital. She graduated from UCLA NP/CNS program in 2017 and completed her Doctorate in Nursing Practice in 2020. She is a board-certified Gerontological Nurse Practitioner. She has worked as a frontline nurse in a med/surg/palliative/EOL unit for 10 years and is working as a Geriatric Clinical Nurse Specialist for past 15 years. She has implemented multiple projects including delirium prevention and management program to improve outcomes of geriatric patient population across the health system. Sigrid Ladores, PhD, FAAN; University of Alabama at Birmingham; Birmingham, Alabama Dr. Sigrid Ladores is a pediatric nurse practitioner, clinical nurse specialist, certified nurse educator, and Fellow of the American Academy of Nursing. She has served in several leadership roles including the Director of the PhD Program and the Co-Director of the BSN Honors Program. She is also a leader in the Philippine Nurses Association of America (PNAA) where she is currently the Co-Chair of the Research Committee and the President of the Alabama chapter. Dr. Ladores earned her BSN and MSN degrees from the University of Pennsylvania and her PhD in Nursing from the University of Central Florida. Shannon Layton, DNP, RN, LICSW, NEA-BC, CNL, CNE,; University of Alabama at Birmingham School of Nursing; Birmingham, Alabama Dr. Layton, is currently an Assistant Professor at University of Alabama at Birmingham School of Nursing where she is the Specialty Track Coordinator for both the Clinical Nurse Leader and Nurse Management of Care Transitions MSN Programs. During her career as a nurse and clinical social worker, she has founded three corporations to deliver treatment services to clients in at risk or under-served areas of the Southeast. Her areas of academic interest include implementation of interprofessional quality improvement (QI) initiatives to optimize transitions of care for patients/Veterans across the health care continuum and development of clinically focused QI teaching strategies. Lucy Leclerc, PhD, RN, NPD-BC; uLeadership; Atlanta, Georgia Dr. Lucy Leclerc is a nurse executive, author, and Chief Innovation and Learning Officer for uLeadership. Her research focuses on healthcare leadership in practice and in academia with the aim to connect leadership behaviors with metrics and outcomes for staff, patients, and communities. She serves on the Editorial Board of the Journal of Nursing Education and has published research in many peer-reviewed journals. Over the years, Dr. Leclerc has led teams in venues from the bedside to the executive director role to tarmacs across the world in the United States Air Force Reserve as an officer and flight nurse. Jennifer H. Ledlow, MSN, RN, CCRN-K, CNL, CNE; UAB School of Nursing; Birmingham, Alabama Jennifer H. Ledlow, MSN, RN, CCRN-K, CNL, CNE obtained her ADN from Central Alabama Community College in 2004. She obtained her BSN and MSN from the University of Alabama at Birmingham in 2014 and 2016, respectively. Jennifer has been employed as a full-time faculty member at the University of Alabama at Birmingham since 2018. She has been the Nursing Simulation Coordinator since 2020 and works collaboratively with undergraduate faculty, graduate faculty, and community partners to develop and facilitate simulation opportunities. Jennifer is a Clinical Nurse Leader passionate about patient safety and improving the nursing work environment. Gloria Loera, DNP, RN, NEA-BC; Texas Tech University Health Sciences Center; El Paso, Texas Dr. Loera has nursing experience both clinically and in leadership. Her clinical background includes women's health and patient educator. She has held various nursing leadership positions. She is a program director for graduate studies at Texas Tech University Health Science Center in El Paso, Texas. She has an interest in civility and leadership studies. Lyn Stankiewicz Losty, PhD, MBA, RN; Walden University; Corolla, North Carolina Lyn Stankiewicz Losty, PhD, MBA, MS, RN has had a strong career in today’s healthcare environment. Starting as a surgical intensive care nurse, she practiced clinically for over 5 years, spent 10 years in executive leadership at Hill-Rom Industries, and culminated her career with 18 years in higher education at the University of Maryland School of Nursing (UMSON) where she served as an associate professor and Director of the Health Services, Leadership, and Management specialty track. Dr. Losty is a contributing faculty member in Walden University School of Nursing’s DNP programs where she teaches and mentors tomorrow’s nurse leaders. Shelly Luger, RN, DNP, NE-A BC; Creighton University; Omaha, Nebraska Dr. Luger is an assistant professor at Creighton University College of Nursing. She is the track lead for the nursing administration and leadership program. Dr. Luger is an evidence- based practice mentor, board certified as a nurse executive advanced leader, and she is preparing for national certification as a leadership coach. Shelly has held several leadership positions in nursing practice and nursing education. Her project interests include empowering nurse leaders to tell their stories, nurse leader burnout, leadership simulation experiences, developing leadership skills in new graduate nurses, complexity science and systems leadership in free and charitable clinics. Giancarlo Lyle-Edrosolo, DNP, RN, CENP, NEA-BC, FAONL; Advocate Christ Medical Center; Chicago, Illinois Dr. Giancarlo Lyle-Edrosolo is the Vice President and Chief Nursing Officer at Advocate Christ Medical Center in Oak Lawn, Illinois. Giancarlo is an inducted Fellow of the American Organization for Nursing Leadership (AONL), a 2020 AONL Nurse Executive Fellow, and a past board member for AONL and the Association of California Nurse Leaders (ACNL). He is an active member of several professional organizations and serves in national/state committees and task forces. Giancarlo has won local, state, and national leadership and public policy awards. He is passionate about leadership development and creating a pipeline of competent nurses to assume emerging roles from the bedside to the board room and beyond. Mithun Mahinda, CCRN, CMC; UCLA Health; Santa Monica, California Critical-Care Board-Certified nurse with six years of clinical experience in a medical intensive care unit. Serves as the education team’s lead educator. Chair of the New Knowledge & Innovations Collaborative Magnet Council. Created an innovative, multimodal evidence-based model using design thinking. Warisara Manuel, RN, MSN; UTHCS Cizik School of Nursing; Texas, Texas Ms. Warisara is a PhD student at UTHealth Cizik School of Nursing studying nursing workforce determinants of health care quality. Gabriela Marcellino de Melo Lanzoni, PhD, RN; Universidade Federal de Santa Catarina; Florianópolis, Brazil Assistant Professor at Nursing Department and Nursing Graduate Program at Universidade Federal de Santa Catarina Adelais Markaki, PhD, APRN-BC, FAAN; University of Alabama at Birmingham; Birmingham, Alabama Dr. Ada Markaki is Professor and Co-Director of the PAHO/WHO Collaborating Center for International Nursing at UAB School of Nursing. As Chair of the Pan American Nursing and Midwifery Collaborating Centers (PANMCC) network, which includes 16 Centers in the Americas region, she empowers and advocates for nursing and midwifery workforce development. An international health systems’ researcher, Dr Markaki studies nursing contributions to primary health care and global health. She is a Fellow in the American Academy of Nursing, and a recipient of the Graduate Dean’s Award for Excellence in Mentorship of graduate students and international scholars. Ligia Neres Matos, Registered Nurse; Pro-Cardíaco Hospital; Rio de Janeiro, Brazil Nurse from the Federal University of Rio de Janeiro (2007). Specialist in heart failure, heart transplantation, and circulatory assistance - LVADs. Member of The International Consortium of Circulatory Assist Clinicians, Master of Science in Nursing and doctoral student in nursing at the Anna Nery Nursing School/UFRJ. Marie McBee, DNP, MSN; UTHealth | The University of Texas Health Science Center at Houston; Houston, Texas Marie McBee brings over 20 years of leadership experience in senior-level administration to the Cizik School of Nursing. She holds a background in administration at the CEO, COO, VP, CNE levels of healthcare, both inpatient and outpatient. Marie has been teaching at all curriculum levels within the school of nursing, BSN, MSN and DNP. She has been a leader in quality improvement projects in patient safety and hand-off communication. Deborah McCrea, EdD, MSN, APRN, FNP-BC,CNS, CNE,CEN, CFRN, EMT-P; UTHealth School of Nursing at Houston; Houston, Texas Debbie McCrea is an assistant professor at UTHealth in Houston where she teaches in the nurse practitioner program. She received her master’s degree in Emergency CNS/Education and completed a postmaster in Emergency/Family Nurse Practitioner program. She was an EMS Clinical Nurse Specialist at the Houston Fire Department. She works prn as a medical case manager for a travel assistance company coordinating care for travelers who experience medical emergencies. She completed an Educational Doctorate (EdD) in Professional Leadership in Health Science Education from the University of Houston where her interest includes instructional technology and educational simulation especially in Mass Casualty Training. Taishayla McKitt is an epidemiologist and data analyst for Nurse Family Partnership of Central Alabama. Caitlin McVey, RN, MBA; UTHCS Cizik School of Nursing; Houston, Texas Ms. McVey is a PhD student at UTHealth Cizik School of Nursing studying nursing workforce determinants of health care quality. Katherine A. Meese, PhD; University of Alabama at Birmingham; Birmingham, Alabama Katherine A. Meese, Ph.D is an Assistant Professor in the Department of Health Services Administration at the University of Alabama at Birmingham. She also serves as the Director of Wellness Research in the UAB Medicine Office of Wellness and Director for the Center for Healthcare Management and Leadership. Dr. Meese has several years of industry experience including working in management within a large academic medical center. She has co-authored two textbooks for organizational behavior in healthcare, as well as numerous book chapters and peer-reviewed articles. Her research interests are in organizational behavior, leadership, well-being, and organizational learning. Sheila Melander, PhD, APRN, ACNP-BC, FCCM, FAANP, FAAN; UK College of Nursing; Lexington, Ky, Kentucky Will not be speaking; First author will do presentation Melissa Miller, PhD, RN, CNOR; Womack Army Medical Center; Fort Bragg, North Carolina MAJ Melissa Miller is an active-duty, Nurse Scientist in the United States Army Nurse Corps. She is a health services researcher with programs of research focusing on staff nurse retention, ambulatory care nurse sensitive indicators, and ambulatory care nursing practice environments. Hadelândia Milon de Oliveira, Prof da Universidade Federal do Amazonas; Universidade Federal do Amazonas; Manaus, Brazil Possui graduação em Enfermagem pela Universidade Federal do Amazonas (2003), mestrado em Saúde, Sociedade e Endemias na Amazônia pela Universidade Federal do Amazonas (2010) e doutorado em Doutorado em Enfermagem na Saúde do adulto pela Universidade de São Paulo (2016). Atualmente é professora associada da Universidade Federal do Amazonas. Tem experiência na área de Enfermagem: atuando principalmente nos seguintes temas: enfermagem, segurança do paciente, sistematização da assistência de enfermagem. Rebecca (Suzie) Miltner, PhD, RN, CNL, NEA-BC; University of Alabama School of Nursing; Birmingham, Alabama Dr. Suzie Miltner joined UAB in 2012. She is also a Nurse Scientist at the Birmingham VA Medical Center. She has extensive clinical and leadership experience in military, private, and VA acute care settings as well as well as experience in nursing education in both academic and organizational settings. She has been a leader in driving quality improvement efforts in several health care organizations including ongoing work as a facilitator for VA improvement teams. Linda Moneyham, PhD, RN, FAAN; University of Alabama at Birmingham; Alabama, Alabama Linda Moneyham is the Senior Associate Dean for Academic Affairs at the School of Nursing, the University of Alabama at Birmingham. Dr. Moneyham holds a BSN degree from Berea College and graduate degrees in nursing from the University of Kentucky (MSN) and Indiana University (PhD), with advanced clinical specialization in community mental health/psychiatric nursing. With more than 30 years of academic experience, Dr. Moneyham is highly regarded for her long-standing program of federally funded research focused on rural and minority populations with HIV/AIDS and other health disparities. Aoyjai P. Montgomery, PhD, BSN; University of Alabama at Birmingham; Birmingham, Alabama Dr. Aoyjai Montgomery is a Scientist I at Department of Epidemiology, School of Public Health, UAB whose expertise is in burnout, work environment, and patient safety among nurses and nurse leaders. She is an expert on data analysis using various data analytic techniques and interpretation, as well as data display; in addition, she has designed electronic surveys using Qualtrics and REDCap. She also has successfully collaborated with the interdisciplinary research team. Furthermore, she has been serving as a data analyst for many research projects and a statistical consultant for many PhD dissertations and DNP projects. Patricia Mook, MSN, RN, NEA-BC, CAHIMS, FAONL; Advocate Health; Charlotte, South Carolina Patricia Mook, MSN, RN, NEA-BC, CAHIMS, FAONL, is Vice President of Nursing Operations for Atrium Health. Patricia is a popular mentor who encourages innovation. She has published multiple articles on mentoring nursing leaders is a passionate national speaker. She has previously served on the American Organization for Nursing Leadership (AONL) Board of Directors and is the current Development Chair for the AONL Foundation. Her goal is to develop executive nurse leaders across our nation. She was recently recognized as a Great 100 Nurse leader in North Carolina. Patricia is an AONL Fellow and was named the 2023 AONL Exemplary Leader. Randy Moore, DNP, RN; United States Department of Veterans Affairs; Birmingham, Alabama Dr. Moore seeks to improve knowledge dissemination to nursing students on Veterans’ related health issues. The special population group of Veterans and their family members has certain conditions, which while not unique to Veterans, do occur with increased frequency. Special conditions include post-traumatic stress disorder (PTSD; recognition and treatment), mild traumatic brain injury (mTBI), women Veterans, environmental exposures, palliative care for Veterans, homelessness, and Veteran suicide. There are over 24 million Veterans in the U.S. Denise Morris, PhD, RN; University of West Georgia; Carrollton, Georgia Denise Morris, PhD, RN is an Assistant Nursing Professor at the University of West Georgia. Dr. Morris has significantly contributed to the field of nursing for nineteen years, specifically as it relates to diversity, equity, and inclusion. The University of West Georgia appointed Dr. Morris as one of six faculty to represent the university as a Chancellor Learning Scholar within the university system. She is an active member of the Transcultural Nursing Society, as well as a board member of the Georgia Association for Nursing Education; recently also serving on the board of the PiNu chapter of Sigma. Joysline Ndungu, DNP, RN; Wellstar Paulding Medical Center; Hiram, Georgia Dr. Joysline Ndungu is the Assistant Nurse Manager of the IMCU unit at Wellstar Paulding Medical Center. Dr. Ndungu received her ASN from Chattahoochee Technical College in 2011, BSN, MSN and her Doctorate from Chamberlain University. Dr. Ndungu also holds a certification in Progressive Critical Care Nursing. Dr. Ndungu has experience in long term care nursing, cardiac nursing, and has supported new graduate nurses as residency coordinator. Dr. Ndungu is a board member of Sigma Mu Phi – At large chapter, and is a member of AACN, ANA and GNA. Heather Nelson-Brantley, PhD, RN, NEA-BC; University of Kansas; Kansas City, Kansas Heather Nelson-Brantley, PhD, RN, NEA-BC, is VP of Research for ALSN, and Associate Professor and Leadership Program Director at the University of Kansas School of Nursing. Dr. Nelson-Brantley uses qualitative, quantitative, mixed methods, and implementation science approaches to study the nursing workforce, nursing practice environment, organizational change, and cancer care delivery. She has led or co-led several federal, foundation, and association funded studies, including Co-PI of this study. She is well published in nursing leadership science. Nga Nguyen, MPH, MAiL; Arcadia, California Nga Nguyen, MPH, MAiL, is a public health scholar from Vietnam. She holds a Bachelor of Public Health from Hanoi University of Public Health (Vietnam) and two Master’s degrees, Master of Public Health concentration on Health Policy and Administration, and Master of Arts in Leadership from Azusa Pacific University (USA). Nga has cross-culture administrative experience in providing strategy development and training for healthcare workforce through US non-profit organizations in Vietnam. She has a strong passion to develop her health policy competencies focusing on healthcare workforce development and improve healthcare quality programs. Charlene Noble, MED, PHR; Wellstar Health System; Marietta, Georgia Consultant, Leader Development, for Wellstar Health System, where she is responsible for the implementation of key programs, including a new system-wide Leader Fundamentals and Aspiring Leader programs. She has been with Wellstar for 11+ years, starting as Talent Acquisition Team Lead, then Manager of Centralized Onboarding. She then moved into Organizational Learning as lead facilitator/training coordinator for New Employee Orientation, and most recently worked with the Organizational Effectiveness team as Program Manager for Mentoring and Career Development. Charlene has an extensive background in the HR and Learning spaces, including previous positions with Walt Disney Parks and Resorts and LexisNexis. Nikhil Padhye, PHD; UTHCS Cizik School of Nursing; Houston, Texas Dr. Padhye received his PhD in physics from the University of Texas at Austin and he is currently Professor with tenure at Cizik School of Nursing at UTHealth Houston. Dr. Padhye teaches courses in statistics and data science. Graciele Oroski Paes, Associate Professor; Universidade Federal do Rio de Janeiro; Rio de Janeiro, Brazil Postdoctoral by the Faculty of Nursing, Physiotherapy and Podology of the University of Seville - Spain (2014). Ph.D. in Nursing from the Anna Nery School of Nursing at the Federal University of Rio de Janeiro EEAN/UFRJ (2009-2011). She is a Associate Professor in the Fundamental Nursing Department and Permanent Professor in the Postgraduate Program in Nursing. She has supervised Master's and Doctoral degrees at UFSC since 2014. Joy Parchment, PhD, RN, NEA-BC, CPDC; University of Central Florida; Orlando, Florida Joy Parchment, PhD, RN, NEA-BC, CPDC is an Assistant Professor at the University of Central Florida College of Nursing and a member of the ALSN Research Committee. Dr. Parchment uses quantitative, qualitative, and mixed methods approaches to study the nursing practice environment, nursing workforce, nurse leader roles, and diversity, equity, inclusion and belonging. She has led and co-led association funded studies, is lead creator of this EBP leadership resource, and publishes on nursing leadership science. In addition to her academic practice, Dr. Parchment serves the nursing profession by influencing, mentoring, and coaching nurse leaders to drive and sustain outcomes. Patricia A. Patrician, PhD, RN, FAAN, Professor and Rachel Z. Booth Endowed Chair in Nursing at the University of Alabama at Birmingham (UAB) School of Nursing in Birmingham, Alabama, joined the UAB faculty after a 26-year career in the U.S. Army Nurse Corps, retiring as a Colonel. Currently, she mentors nursing students in the PhD and Executive DNP Programs, and interprofessional post-doctoral fellows in the VA Quality Scholars program. She conducts research on the nursing workforce and nursing’s contributions to patient safety and quality care outcomes, as well as interventions to assist in the post-pandemic psychological recovery of nurses. Roberta Pawlak, PhD, RN, NEA-BC; University of Wisconsin - Madison; Madison, Wisconsin Roberta Pawlak is a Clinical Professor of Nursing and population lead for the Systems Leadership & Innovation DNP at the University of Wisconsin-Madison. She received a MS degree in Nursing Administration, and a PhD in Nursing, and has held several leadership positions in health services. Dr. Pawlak maintains the ANCC Nurse Executive – Advanced Board Certification and has served on the Board of Directors for the Association for Leadership Science in Nursing (ALSN), Sigma, and Wisconsin Nurses’ Association (WNA) Public Policy Council. Her key interests lie in the areas of leadership, health policy, quality & safety, innovation and strategic & adaptive change in health systems. Terri Poe; Birmingham, Alabama Terri Poe is the Senior Associate Vice President and Chief Nursing Officer (CNO) for the University of Alabama Hospital (Birmingham). Prior to her role as the CNO, she was the Administrative Director for Emergency Services and has served as a nursing leader for over 3 decades. Anne Pohnert, DNP, BSN, FNP-BC, RN; MinuteClinic CVS Enterprise; Woonsocket,, Rhode Island Anne Pohnert is an Advanced Practice Registered Nurse, board certified as a Family Nurse Practitioner for over 20 years. She currently serves as the Lead Director of the Clinical Quality for MinuteClinic, a national convenient care organization with over 1,100 clinics in 36 states and the District of Columbia. Anne leads the national MinuteClinic Clinical Quality program, including clinical quality improvement initiatives, quality measurement, monitoring and quality dashboard development, Joint Commission Ambulatory Care Accreditation, clinical quality reviews and clinical policies and procedures.Anne played a key role in MinuteClinic’s successful designation as an ANCC Pathway to Excellence Organization in 2019. Shea Polancich; Birmingham, Alabama Shea Polancich, PhD, RN, FAAN has been practicing in quality and patient safety for almost 20 years. She is currently an Associate Professor and Assistant Dean at the University of Alabama at Birmingham (UAB) School of Nursing with a primary practice at the UAB Medical Center, Birmingham, Alabama specializing in nursing improvement, innovation, and analytics. Formerly, her roles included the Director for Quality and Patient Safety at Vanderbilt University Medical Center, Director of Data Analysis and Measurement at Texas Health Resources, NIH/NINR research intern, and health policy fellow at George Mason University. She has served on 2 NQF panels. Angela Prestia, PhD, RN, NE-BC; ALSN President, Florida Atlantic University, Case Western Reserve University; Tequesta, Florida Dr. Angela Prestia has devoted her professional nursing career to leadership. Her life’s work, grounded in experience, has resulted in mentorship, research, and authorship of over 50 articles. She is currently faculty at Florida Atlantic and Case Western Reserve Universities. Her nursing leadership career was in practice, as Chief Nursing Officer at 2 facilities. Quality, safety, and staff well-being were a priority. She holds a PhD from Florida Atlantic University. She is ANCC board certified- nurse executive. She currently serves as President for The Association of Leadership Science in Nursing. Kemi Reeves, MSN, RN, GNP-BC; UCLA Health; Los Angeles, California Kemi Reeves, MSN, RN, GNP-BC is a Dementia Care Specialist for the UCLA Alzheimer's and Dementia Care Program and volunteers as an Assistant Clinical Professor at the UCLA School of Nursing. She serves as a lecturer and clinical preceptor, mentoring students specializing in the Adult-Gerontological Nurse Practitioner Program. Kemi is one of the founding members and inaugural chair of the Unity in Diversity Council. This nursing professional governance council implements initiatives to establish an authentic environment of equity, diversity, and inclusion for patients, trainees, and staff. Kemi's areas of clinical interest include integrating cultural humility into healthcare, dementia, and transitions of care. David Reinhart, DNP, MBA, RN, CNOR; 550 Peachtree Street; Atlanata, Georgia David Reinhart DNP, MBA, RN, CNOR is the Director of Education for Procedural Residency Programs for Emory Healthcare System. He has been a perioperative nurse for 36 years. His experience progression started with his role as a nurses’ aide, surgical tech, staff nurse, Supervisor of nursing, Manager of nursing, and service line Director of nursing. Reinhart is a member of AORN Northwest Georgia Chapter 1107. He is a member of ANA, GNA, and Sigma Theta Tau. He is currently serving on the national AORN Nominating Committee and participates in the AORN Executive Roundtable meetings. Lorie Rhine, MSN, RN, NE-BC; UNC Health Rex; Raleigh, North Carolina Over 40 years nursing experience from LPN to RN to CNS to CNO. Has led several nursing organizations through many changes. Known for implementation strategies. Stacie Roberts, MSN, RN is the Education Coordinator for the Postanesthesia Care Unit and Preoperative holding area at Emory University Hospital. She has 12 years of nursing experience with 8 of those years in perioperative nursing, as well as, nursing academic didactic and clinical instructor for 3 years. Stacie’s contribution to the development of the perianesthesia nurse residency program has been instrumental to its success. She serves as a lead instructor of classroom and clinical experiences. Stacie is a member of the American Society if Perianesthesia Nurses, The Georgia Association of Perianesthesia nurses and the Emory Surgical Alliance mission group. MARA REGINA ROSA RIBEIRO, Profa da Universidade Federal do Mato Grosso; Universidade Federal do Mato Grosso; Cuiabá, Brazil Graduação em Enfermagem e Obstetrícia pela Universidade Federal de Mato Grosso (1981), Especialização em Gestão de Hospitais Universitários Federais no SUS e em Qualidade em Saúde e Segurança do Paciente. Mestrado em Enfermagem pela Universidade de São Paulo (1995), Doutorado em Ciências na Escola de Enfermagem da USP - Universidade de São Paulo. Professora da Universidade Federal de Mato Grosso, Líder do Grupo de Pesquisa GEFOR - Gestão, Educação e Formação em Saúde e Enfermagem. Orientadora nos Programas de Pós-graduação em Enfermagem - FAEN / UFMT. Integra a RIIEE - Rede Iberoamericana de Investigação em Educação em Enfermagem. Linda Roussel, Ph.D; UTHealth | The University of Texas Health Science Center at Houston; Houston, Texas Dr. Roussel served on the Improvement Science Research Network (ISRN) as Steering Committee member at the University of Texas Medical Center San Antonio engaging in research on operational failures (STAR-2) in healthcare systems. She is currently a member of a research team from the University of Alabama Birmingham investigating methodological potentials and advantages of mixed methods research design for knowledge translation. Dr. Roussel has also developed, managed, and coordinated Executive Nursing Leadership, Clinical Nurse Leader (CNL), and DNP academic programs. Asiah Ruffin, BSN, RN; University of Alabama at Birmingham; Birmingham, Alabama Asiah Ruffin is a registered nurse and a PhD student at the University of Alabama at Birmingham School of Nursing. Her emerging program of research focuses on nursing workforce issues. She is specifically interested in better understanding the association between nurse manager work complexity and patient and organizational outcomes, aiming to create more ideal job designs and work models for nurses and nurse managers in acute settings. Susan Rux, PhD, RN, ACNS-BC, CNE, CPCC, CPRW, FACHE, LNCC, NEA-BC, NPD-BC, OCN, PHN, PNAP; Temple University Health System; Philadelphia, Pennsylvania Dr. Susan Rux is an award-winning nurse leader with greater than 28 years of diverse nursing experience. She is the Associate Vice President, Nursing Education & Professional Development/Innovation with Temple University Health System. Previous professional roles include serving as Dean of Academic Affairs, Chief Nursing Officer, Program Director of Nursing, Associate Professor, and Clinical Nurse Specialist. Her research on preventing incivility in the nursing workplace has received international awareness. Maria Aparecida Pereira Dos Santos Santana, RN; Universidade Federal do Rio de Janeiro; Rio de Janeiro, Brazil Master Student at Anna Nery Nursing School. Head nurse of the Intensive Care of the Clementino Fraga Filho University Hospital/Universidade Federal do Rio de Janeiro. Michelle Santizo, MSN, PHN, RN; University of California, Los Angeles; Los Angeles, California Michelle Santizo is one of the original members that spearhead the creation of the Unity in Diversity Council (UID) at UCLA Health in Nursing the year of 2020 where injustice and racism within our country were at the forefront of our lives. Aside from serving the UID, Santizo focuses her professional development in community, specifically serving the marginalized, low-income, and the homeless population. She hopes to bridge her expertise in health care policy development while engaging stakeholders at the local and national level. José Luis Guedes Santos, Assistant Professor; Universidade Federal de Santa Catarina; Florianópolis, Brazil Ph.D. in Nursing from the Federal University of Santa Catarina - UFSC (2014), with a sandwich period at the Kent State University College of Nursing (USA) and earned his Professional Degree in Nursing (RN) at University of Santa Maria - UFSM (2007). He completed a postdoctoral internship at UFSC (2014). He is an Assistant Professor at the Department of Nursing, a Permanent Professor in the Postgraduate Program in Nursing. He is the Sub-coordinator of the Postgraduate Program in Nursing at UFSC. DANIELLE SARAIVA TUMA DOS REIS, Profa da Universidade Federal do Pará; Universidade Federal do Pará; Belém, Brazil Graduação em Enfermagem pela Universidade Federal do Pará - UFPA (2002); Pós-doutorado em Gestão de Enfermagem pela UFSC (2022); Doutorado e Mestrado em Patologia das Doenças Tropicais pelo NMT/UFPA (2019 e 2008); Especialista em Assistência de Enfermagem em Doenças Tropicais pela UFPA (2003); Professora Adjunta IV da Atividade Curricular Enfermagem em Infectologia, da Faculdade de Enfermagem da UFPA; Experiência em Gestão do Cuidado, Preceptoria da Residência Multiprofissional em saúde, Vigilância Epidemiológica, Segurança do Paciente e Metodologias Ativas de Ensino e Aprendizagem. Maria Shirey, PhD, MBA, RN, NEA-BC, ANEF, FACHE, FNAP, FAAN; University of Alabama at Birmingham School of Nursing; Birmingham, Alabama Dr. Shirey is Co-founder of the HRTSA Heart Failure Clinic. She serves as an executive leadership consultant for strategic direction of the HRTSA Clinic. Tedra Smith, DNP, CRNP, CPNP-PC, CNE, CHSE; University of Alabama at Birmingham; Birmingham, Alabama Tedra Smith is an Associate Professor and Assistant Dean for Graduate Clinical Education – MSN Program for the University of Alabama at Birmingham School of Nursing. Dr. Smith has over 20 years of nursing experience based in chronic care of children and their families and nursing education. She serves as the Director of Pediatric Partnerships in collaboration with Children’s of Alabama. Dr. Smith has led numerous initiatives at the local, state, and national level through various organizational leadership positions. She has several publications and presentations on the care of children and their families, teaching innovations, and partnership development. Todd Smith, PhD, MBA, MSHA, RN, NEA-BC; The University of Alabama; Tuscaloosa, Alabama Dr. Smith is an Assistant Professor at the University of Alabama’s Capstone College of Nursing (UA’s CCN). He regularly teaches graduate courses related to leadership, healthcare management, health services delivery systems, and nursing administration. He has published and/or works on numerous research projects related to rural health care delivery systems, leadership, health care administration, health education, and telemedicine. Dr. Smith has also received federal funding from the National Institutes of Health for a research project related to mental health care in dental practice as well as funding from the United States Department of Agriculture for an ambulance-based telemedicine project. Sara Socorro da Silva Silva, Bolsista de iniciação científica; Universidade Federal do Pará; Belém, Brazil Bolsista de iniciação científica PIBIC/UFPA (2023), Monitora da disciplina de Assistência de Enfermagem em Doenças Transmissíveis, Acadêmica do 9° semestre da FAENF/UFPA. Patricia Span, PhD, RN, CPHQ, CENP; Yale New Haven Health; new haven, Connecticut Dr. Span is the Strategy & Learning Specialist at Yale New Haven Hospital Patient Services Administration with primary responsibility for development and oversight of the nursing strategic business plan and nursing communications comprised of the annual report and nursing news. She has extensive experience as a nurse leader in Education, Professional Practice, Quality, Nursing Research as well as organizational customer service strategies. Patricia received her Doctor of Philosophy in Nursing and is Board certified in Executive Nursing Practice from the Association of Nurse Executives and credentialed in health care quality from the National Association of Health Care Quality. M'Lyn Spinks, DNS, RN, CHSE, CNE, FCN; Kennesaw State University; Kennesaw, Georgia M’Lyn K. H. Spinks, DNS, RN, CHSE, CNE, FCN, is an Assistant Professor at Kennesaw State University (KSU). She has over 30 years of clinical experience consisting in NICU, pediatric ICU, and adult care in community settings. Dr. Spinks maintains expertise in didactic and simulation andragogies and investigates accessibility factors of teaching and learning in higher education. Authored book topics include vulnerable populations, trauma-informed educational practices, and instructional strategies. Dr. Spinks also serves her community by counseling individuals in crisis after trauma and offering specialized training sessions to non-medical academic faculty and staff interacting with students with special needs. Dinah Steele, DNP, RN, CMSRN; Emory St. Josephs Hospital; Atlanta, Georgia Dinah Steele is the Director of Nursing Clinical Excellence and Magnet Program at Emory St. Josephs Hospital in Atlanta, GA. She was a co-Investigator of this Clinician Wellbeing Study. Marluci Andrade Conceição Stipp, Full Professor; Universidade Federal do Rio de Janeiro; Rio de Janeiro, Brazil Nurse from the Federal University of Rio de Janeiro (1992), Ph.D. She holds a degree in Nursing from the Federal University of Rio de Janeiro (2000), Post-Doctorate in Nursing from the Federal University of Santa Catarina (2010). Full Professor at the Anna Nery School of Nursing at the Federal University of Rio de Janeiro. She has been advising Master's and Doctoral degrees at EEAN / UFRJ since 2002. She works in nursing teaching and research with an emphasis on nursing care management, mainly in cardiovascular nursing, customer care in chronic health situations and education in health and lifestyle Patricia Stone, DNP, MSN, RN; Adventist Health; California, California Dr. Stone has been dedicated to nursing and quality patient care for 40 years. With a strong clinical background, she has served as a Chief Nursing Officer in both teaching and community hospitals. Since adding the role of contributing faculty, she has focused on her goal to educate and mentor future nurse leaders. Evan Talton, MSHA, MBA, RN; Children's Healthcare of Atlanta; Georgia, Georgia Evan’s experience encompasses critical care nursing as well as leadership roles in hospital operations and practice management. His experience has allowed him opportunities developing strategies to streamline operations, enhance patient care outcomes, and improve patient experience in various healthcare settings. He is committed to making a positive impact in the healthcare industry and improving the lives of patients and healthcare professionals alike. Lindsey Tarasenko, PhD, RN; Children's Hospital of Colorado; Aurora, Colorado Dr. Tarasenko is a Children’s Hospital Colorado Nurse Scientist, an Assistant Professor at the University of Colorado College of Nursing, and faculty at the Watson Caring Science Institute. She has experience as an adult and pediatric clinician and as a Magnet Program Director. She graduated from CU Nursing in 2019 with a PhD focusing on healthcare systems. As a nurse scientist, Dr. Tarasenko has dedicated her research to improving the nursing practice environment for nursing clinicians and nurse leaders through mixed methods research and psychometric testing. Keri Thomas, MSN, RN, FNP-C; UAB Hospital Nursing Services; Birmingham, Alabama Keri Thomas, MSN, RN, FNP-C has been a registered nurse in the state of Alabama for 15 years. She began her nursing career in the Neurosurgical ICU at UAB Hospital. Seeking to further her knowledge, she enrolled and obtained a MSN from UAB specializing as a Family Nurse Practitioner in 2012. Her passion for neurosurgery and education led her to the Nursing Professional Development Specialist role in the Neuro ICU. A desire for administering safe, high-quality care led to the opportunity to receive a certification in Quality and Safety from UAB's School of Public Health Professions. She currently serves as the Nurse Manager in the Unit for Neurosciences Nursing where she has the opportunity to combine her passions for providing evidence-based care and educating others. Keri hopes to utilize her strengths and passions to continue to progress nursing care. Liana Amorim Correa Trotte, Assistant Professor; Universidade Federal do Rio de Janeiro City: Rio de Janeiro; Rio de Janeiro, Brazil Nurse from the Fluminense Federal University, Ph.D. in Nursing from the State University of Rio de Janeiro. She is an Assistant Professor at the Nursing Methodology Department of the Anna Nery School of Nursing (UFRJ). She has been advising Master's and Doctoral degrees at EEAN / UFRJ since 2021. She works in nursing teaching and research, emphasizing nursing care management, mainly in cardiovascular nursing and palliative care. Sharon Tucker, PhD, APRN-CNS, NC-BC, FNAP, FAAN; Ohio State University; Columbus, Ohio Dr. Sharon Tucker is the Associate Dean for Health Promotion and Well-being and Director of the Center for Well-being and Prevention at The Ohio State University (OSU). She is also the Grayce M. Sills Endowed Professor of Psychiatric Mental Health Nursing and practices, studies, and teaches behavioral and mental health interventions to promote health, prevent disease, and reduce stress among working populations and college students. Having served as a leader in clinical settings for 15 years, she is an expert in evidence-based practice, quality improvement, and change management, and directs the Implementation Science Core of the OSU Fuld EBP Institute. Julia Turner, JD, MBA, BSN, CPHRM; University of California San Francisco; San Francisco, California Julia Turner started her career as a nurse in the emergency department in a Level I trauma center. She attended law school part-time while working as a nurse in the ICU and then worked to defend medical providers and hospitals including working for The Ohio State University Wexner Medical Center managing claims. Julia is now the Risk Manager at UCSF Benioff Children’s Hospital in Oakland, California. Todd Tussing, DNP, RN, CENP, NEA-BC; The Ohio State University; Columbus, Ohio Todd E. Tussing, DNP, RN, CENP, NEA-BC has over 35 years of nursing experience. He has held the titles of nurse manager, director, and administrative director. Originally a diploma nurse, he completed his BSN (Capital University), MS and DNP (Wright State University). He currently holds dual certifications in nursing administration. Has taught in pre-licensure program, RN-BSN program, and Master of Science program. He currently teaches in the Master of Healthcare Innovation and DNP programs at OSU College of Nursing. Courses taught include: Leadership, Health Policy, Quality Improvement, Best Practices in Organizational Operations, Organizational Culture, and Innovation in High Performing Organizations. Sonia Udod, RN,PhD; University of Manitoba; Winnipeg, Canada Dr. Sonia Udod has an active program of research on healthcare leadership and expertise in qualitative research. As Co-PI for Creating and Translating Evidence for Nursing LEADership and Health Services (Lead Outcomes Research), my research program focuses on nurse leader development critical to supporting high-quality healthcare environments leading to quality nurse, patient, and organizational outcomes. I serve as the Chair of the Leadership, Management and Policy in the Nursing Education Interest Group of the Canadian Association Schools of Nursing (CASN), and served as the International Director, Association of Leadership Science in Nursing. Lynn Varagona, PhD, MBA, RN; Kennesaw State University; Kennesaw, Georgia Dr. Lynn Varagona is an Associate Professor of Nursing at Kennesaw State University, a Board Certified Psychiatric-Mental Health Clinical Nurse Specialist, and a licensed Psychologist. She holds a PhD in Community/Organizational Psychology from Georgia State University, an MBA with a concentration in the Business of Health Care from Emory University, a Master of Science in Nursing from Yale University, and a Bachelor of Science in Nursing from the University of Florida. Dr. Varagona has published her research on creating healthy practice environments through team virtuousness and perceived trustworthiness in major nursing journals and presented at numerous international conferences. Sherri Wall, MSHA BSN RN CNOR; UAB School of Nursing; Birmingham, Alabama Sherri Wall is a second year DNP Student at University of Alabama Birmingham. She currently serves as the Senior Director for UAB Medicine Heart and Vascular Center in Birmingham Alabama. Experienced Operational consultant for Cardiovascular, Perioperative, and Endovascular services. Forty years’ experience in healthcare and twenty plus years in professional leadership with extensive knowledge in strategic planning in healthcare operations and financial performance. Experienced in team building and interprofessional collaboration. Credentials include Master of Science (MS) focused in Healthcare Administration Management and Certified Lean Six Sigma Green Belt. Results driven with a strong record of accomplishment for performance. Charlotte Walton, RN, MPH; Birmingham, Alabama Charlotte Walton is a nurse supervisor with Nurse Family Partnership of Central Alabama. Cathy Ward, Ph.D, RN, NEA-BC; University of Alabama at Birmingham; Birmingham, Alabama Cathy Rodgers Ward, PhD, RN, NEA-BC Dr. Cathy Rodgers Ward is currently Executive Clinical Scholar in Residence at the University of Alabama in Birmingham in the Executive Doctor of Nursing Practice Program. She has a stellar record of leadership as a previous Chief Nursing Officer at the UCLA Ronald Reagan Medical Center, an academic medical center consistently ranked in the top five in the nation, and as a university professor at the graduate level. Dr. Ward holds a proven track record for improving patient outcomes, nurse engagement and student success. Susan Weaver, PhD, RN, CRNI, NEA-BC; Hackensack Meridian Health; Neptune, New Jersey Susan H. Weaver, PhD, RN, CRNI, NEA-BC, a nurse scientist at Hackensack Meridian Health Ann May Center for Nursing, has more than 30 years of nursing leadership experience. Her program of research focuses on the nursing workforce, particularly administrative supervisors and clinical nurses who work the night shift, and improving outcomes. Recently she has completed a qualitative systematic review on the experiences and perceptions of nurses working night shift. Dr. Weaver and Dr. Wurmser received funding for the study reported in this abstract submission from the ALSN Versant Center for the Advancement of Nursing Pilot Award in 2022. Dr. White-Williams is Co-founder and current Senior Director of the HRTSA Heart Failure Clinic. She has executive leadership oversight of the daily operational, financial, and strategic direction of the HRTSA Clinic. Polly Willis, MSN, NE-BC, PCCN; Emory University Hospital; Atlanta, Georgia Polly Willis is the Director of Nursing Clinical Excellence and Magnet Program at Emory University Hospital in Atlanta, GA. She was a co-Investigator of this Clinician Wellbeing Study. Lisa Woodely, PhD, MSN, RN, CNE, CHPN; School of Nursing, UNC-CH; Chapel Hill, North Carolina Dr. Woodley is passionate about educating future generations of nurses and nurse educators in a way that demonstrates the art and science of nursing and nursing education. She serves as a mentor for students and junior faculty. Her scholarship and service echo her passion for inclusive nursing education and the importance of global education for nursing students. She has presented at local, regional, statewide, national and international conferences and has cherished her work with undergraduate nursing students for over 30 years. Theresa A. Wurmser, PhD, MPH, RN, NEA-BC; Hackensack Meridian Health; Neptune, New Jersey Teri Wurmser, PhD, MPH, RN, NEA-BC has over 45 years of experience in nursing and health care. Dr. Wurmser currently serves as Vice President of Nursing Research, Grants and Academic Affairs, Hackensack Meridian Health, Ann May Center for Nursing and is the founding Dean of the Georgian Court-Hackensack Meridian Health School of Nursing. She has been the project director for multiple, successful HRSA Workforce and Nurse Education, Practice, and Retention Program grants and is an experienced leader, grant writer and researcher. |
Abstracts Ordered by Abstract ID (listing first author only) 5-R. Retelling the Stories: Registered Nurses’ Lived Experiences of Peer-to-Peer Incivility in the WorkplaceSusan Rux, PhD, RN, ACNS-BC, CNE, CPCC, CPRW, FACHE, LNCC, NEA-BC, NPD-BC, OCN, PHN, PNAP; Temple University Health System; Philadelphia, Pennsylvania 10/28/2023, 3:10pm - 4:00pm, Breakout: 6 The purpose of this qualitative study was to explore registered nurses’ lived experiences of peer to peer incivility in the workplace. An aim of this study was to understand the participants’ experiences of peer-to-peer incivility in the workplace, its effect on patient safety and nursing job satisfaction and retention. 6-R. Impact of the Doctor of Nursing Practice Degree: A Look Back from the Beginning of the First DNP Program to Today Debra Hampton, PhD, MSN, RN, NEA-BC, CENP, FACHE, FAONL; UK College of Nursing; Lexington, Ky, Kentucky 10/29/2023, 3:00pm - 3:50pm, Breakout: 16 Background: The Doctor of Nursing Practice degree (DNP) prepares nurses to lead improvements in outcomes and translate evidence into practice. Multiple studies have been focused on the impacts DNP nurses make and demonstrated that DNP nurses have made extensive organizational impacts, but gaps still exist in quantifying the value of DNP education and in educating about what DNP prepared advanced practice nurses can do that is different than MSN educated nurses. Purpose The purposes of this presentation will be to illustrate the value one college’s DNP graduates have brought to the profession and show how DNP projects can bring value to the profession and to organizations within which projects are conducted. Methods A cross-sectional survey design was employed for this mixed-methods DNP assessment that included graduates who spanned over 20 years (2005 to 2021). The population included 448 DNP graduates, but contact information was only available for 348. The survey consisted of demographic items, items focused on DNP impact, outcomes from the DNP project, and open-ended descriptive items. Participants included graduates who worked in hospital, academic and various other settings. Results Of the 348 participants in the study, ninety responded to the survey and thus made up the participant group. Over 84% of participants reported that the DNP helped them stand out as a leader and 86% stated the DNP impacted career advancement. Post BSN to DNP graduates perceived less value from the program than did post-MSN students. Participants reported the top achievements from the DNP program to be career advancement, improved patient care outcomes, evidence-based initiatives, and growth as a leader. Increased professional credibility was also mentioned by several participants. Forty eight of 90 students validated that their DNP project helped to influence or contribute to practice as an advanced practice nurse and one stated their project “changed policy”. Examples of the impact from a DNP degree included: “ My DNP education has opened several doors for me. It gave me a good foundation for success. . . .” “I have countless job opportunities… The sky is the limit for me...I have so many options and that is the blessing of my DNP” Conclusion The findings from this study supported the AACN 2022 report which indicated that DNP graduates impact patient and organizational outcomes by the translation of evidence into practice and through applying leadership skills in unlimited situations/settings. The DNP made graduates stand out as a leader and illustrated the broad return on investment that employing DNP graduates can bring. However, more study is needed to differentiate or illustrate how DNP education results in a different level of outcome impact. Additionally, DNP education merits consideration by nursing leaders outside of the United States since most international countries with doctoral level nursing programs have PhD’s or Professional Doctoral degrees. At the same time that colleges of nursing across the United States begin to assess the advanced level competencies of DNP graduates, as outlined in the new 2021 Essentials, quantifying outcomes from DNP programs needs to be a stronger focus. 7-EBP. Models and Methods for Competency Validation in an Online Graduate Leadership Course Debra Hampton, PhD, MSN, RN, NEA-BC, CENP, FACHE, FAONL; UK College of Nursing; Lexington, Ky, Kentucky 10/29/2023, 12:00pm - 1:50pm, Poster Session Background: The new AACN Essentials (2021) include 205 sub-competencies that outline learner expectations at the advanced nursing education level. The goal of the new Essentials is to move nursing education to a competency-based system focused around the demonstration of what students can do with the knowledge they have. Thus, the new Essentials address the outputs of the educational experience. AACN defines competency-based education as “a system of instruction, assessment, feedback, self-reflection, and academic reporting that is based on students demonstrating that they have learned the knowledge, attitudes, motivations, self-perceptions, and skills expected of them as they progress through their education.” (2023). How to validate competency in the performance of specific clinical skills is less complex than is validating competency for less quantifiable leadership skills, such as having an effective critical conversation, successfully leading a team, etc. Further, determining how to validate competency in an online educational environment offers multiple complexities. Purpose: The purposes of this presentation will be to present a competency validation model that illustrates the level at which competency occurs and to present examples of assignments that can be used in a leadership course to validate competency for specific advanced nursing education level sub-competencies. Methods to Validate Competence: Miller’s Pyramid of Clinical Competence and Bloom’s Taxonomy Revised demonstrates levels at which competency occurs. According to Miller’s model, the cognitive aspects of competence occur at the “Knows” (knowledge) and “Knows How” (application of knowledge) levels. Skills competency occurs at the “Shows” level where individuals can demonstrate how to do things or at the “Does” level (clinical performance) where individuals perform tasks; these two levels represent behavioral aspects of competence (Witheridge et al, 2019). Based on Bloom’s Taxonomy, “Creating” is synonymous with the “Does” level of Miller’s model. Two assignments were created within an Executive Leadership DNP course that allow for the validation of specific essentials sub-competencies at the “Shows” level. These included: “How Do I Show Up as a Leader” where students create a plan for beginning a new Chief Nursing Officer position and “How to Best Prepare Our Organization for Catastrophic External Events as a Strategic Leadership Team”. Results: As demonstrated by experience in past courses, students verbalize immense value from completing these two assignments. Examples of Essentials sub-competencies that allow for competency validation through these assignments include: 7.3e, Apply innovative and evidence-based strategies focusing on system preparedness and capabilities; 10.1d, Evaluate the workplace environment to determine level of health and well-being; and 10.3, Demonstrate leadership skills in times of uncertainty and crisis. Conclusion: Assignments focused around responding to realistic practice scenarios can be effective methods of validating that a student has specific nursing leadership related competencies. Although the traditional methods of validating competency, directly observing someone’s performance (the “Shows” or “Does” levels) are the first methods that comes to mind for competency validation, nursing leaders will need to use multiple innovative methods in online nursing leadership degree programs to measure competency. 8-R. COVID-Related Burnout: Nurses' Perspectives and Priorities Roberta Kaplow, Ph.D., APRN-CCNS, AOCNS, CCRN, FAAN; Emory University Hospital; Atlanta, Georgia 10/29/2023, 12:00pm - 1:50pm, Poster Session Purpose: The purposes of this study were to determine whether positive work environments affect clinician wellbeing and identify priority interventions to improve clinician wellbeing. This study was designed to determine the potential benefit of modifying the factors for hospitals to impact patient outcomes. Relevance/Significance: The COVID-19 pandemic became one of the leading causes of death in the US and worldwide and exacerbated burnout among healthcare professionals. This resulted in negative collateral implications for the stability of the clinician workforce. A Clinician Wellbeing study (CWS) was launched in two Magnet-designated hospitals. The CWS was part of a multi-site collaborative project led by the Center for Health Outcomes and Policy Research at the University Of Pennsylvania School Of Nursing. Implementation: A cross sectional observational study design was implemented. Data were collected through anonymous surveys of 708 registered nurses (RNs) and advanced practice providers (APPs) working in two Magnet hospitals in the southeastern United States. Eight surveys were completed by each participant. Outcomes/Results: Clinicians’ self-reported level of burnout was higher for both RNs and APPs at Hospital A than Hospital B including intent to leave and dissatisfaction with their jobs. RNs and APPs self-reported their overall health to be good or excellent they reported sleep quality as fair. Both groups in Hospitals A and B indicated that they experienced anxiety, depression, and stress. The APPs reported a higher percent that their work did not leave enough time for personal and family life. Data also indicated that the primary work environment concern was related to inadequate numbers of nurses to care for patients. Conclusion: The data illuminated opportunities for the two hospitals to employ continuous improvement interventions to positively transform the work environment. 9-R. Does Zip Code Predict Patient Outcomes? Roberta Kaplow, Ph.D., APRN-CCNS, AOCNS, CCRN, FAAN; Emory University Hospital; Brookhaven, Georgia 10/28/2023, 3:10pm - 4:00pm, Breakout: 5 Project Overview: The purpose of this study was to evaluate the relationships among Sequential Organ Failure Assessment Score, race, gender, payer, zip code of primary residence, and patient outcomes in patients with COVID-19. Background: There are reported disparities in healthcare outcomes of minority populations. Some etiologic factors include race-associated comorbidities, socioeconomic status, and lack of access to health care. Disparities have been further intensified due to COVID-19 and its associated sequelae. Black, indigenous, and people of color (BIPOC) and Hispanic people have reported higher infection rates and complications of COVID-19. Hospitalization and death rates for BIPOC are higher than White persons. Determining if specific demographic variables can potentially impact patient outcomes is essential so they can possibly be mitigated. The Chief Nursing Officer approved conduct of this study. She appreciated the need to continue to identify factors that impact patient outcomes so that appropriate interventions may be implemented in our healthcare system. Intervention Detail: A retrospective chart review of 100 patients with COVID-19 admitted to an ICU of an academic medical center in the southeast was performed. Patients were admitted with acute hypoxic respiratory failure. Zip code of the patient’s primary residence was the main demographic variable; other variables reported to impact patient outcomes in the literature were also evaluated. Outcomes and Impact: Patients with organ failure had a longer length of stay in the ICU. African American patients and those with Medicare/Medicaid, compared with all other payers, had the shortest time to development of organ failure. There were no statistically significant differences between zip code of primary residence and length of stay, days until organ failure, or patient survival. While disparities in healthcare outcomes exist in minority populations and those of lower socioeconomic status, this trend did not manifest in our patient cohort. 10-ASP. Preparing international nurse researchers: an equitable and inclusive PhD program initiative Adelais Markaki, PhD, APRN-BC, FAAN; University of Alabama at Birmingham; Birmingham, Alabama 10/28/2023, 2:10pm - 3:00pm, Breakout: 1 Problem, Significance, Rationale Global disparities in nursing education have come to the forefront since the COVID-19 pandemic and the release of the Global strategic directions for nursing and midwifery 2021-2025 report.1 Research-intensive nursing programs are beginning to focus on doctoral education through the lens of diversity, equity, and inclusion (DEI). Adopting DEI perspectives can ameliorate disparities’ impact by preparing the next generation of international nurse researchers and leaders. Purpose, Project Goals To describe the structure, process, and outcomes of an innovative international PhD program initiative led by a School of Nursing (SON) in the United States. This initiative aimed to diversify the PhD student body and expand opportunities for research-focused doctoral education. Project goals included removing barriers in international PhD student recruitment, ensuring academic success, and strengthening retention. Methods, Collaboration, Implementation Structure: Through a cross-campus academic-service partnership, SON instituted systematic recruitment, comprehensive evaluation of international applicants, and continuous support of matriculating students. Partnership with INTO - an organization specializing in raising student body diversity and expanding international opportunities for faculty - offered access to English language programs, academic advising, tutoring, orientation, cultural and other student-life enrichment activities. Within SON, the PhD program Office and the Office of Global Partnerships spearheaded recruitment, selection, onboarding, and support efforts. Process: Through collaborative planning and evaluation meetings, we established admission criteria based on language proficiency and transcript equivalency review processes. Upon review of the application portfolio, an interview invitation or a declination letter was generated. Qualified applicants were offered direct-entry, one-semester, or two-semester pathways admission, based on language proficiency. Pathways allowed for seamless progression into the PhD program while receiving immersive training in Academic English. International students met with INTO tutors weekly, as well as with faculty mentors. They also participated in monthly PhD student Town Hall meetings, PhD student-led DEI group, and an International PhD Student Group mentoring community. Results Outcomes: Since 2019, twelve international students were admitted to the program, compared to only one prior to initiative implementation. Of the 12 students, four enrolled through INTO pathways, four came from low or middle income countries, and nine received full funding with stipend. To date, there has been no attrition. Two students have successfully graduated from the program and assumed post-doctoral fellowships. All current students are on-track and excelling in their studies. Implications: Recruiting and admitting international PhD students requires significant time, effort, funding, and dedicated university resources. Students must actively engage with and utilize all support services to optimize their academic successes and adjust to life in another country. Raising awareness and skill levels in cultural sensitivity and inclusivity is paramount for PhD faculty and staff. Conclusion There is renewed interest in addressing nursing education disparities by bolstering international nurses receiving a research-focused PhD education in the United States.2 Our early findings show that an academic-service partnership facilitates successful recruitment and matriculation, while decreasing the risk of attrition among international PhD students. Systematic, ongoing support for an equitable and inclusive initiative that prepares the next generation of international nurse researchers is essential. Shelly Luger, RN, DNP, NE-A BC; Creighton University; Omaha, Nebraska 10/29/2023, 10:10am - 11:00am, Breakout: 8 Background: Health care challenges are endless. These challenges have led to nurse leaders feeling overwhelmed with the amount of work and responsibility of leading teams in the complex healthcare environment. In addition, as humans nurse leaders are fallible. Checklists can assist in maintaining focus on mission critical elements. Dr. Angela Prestia has developed the Nursing Leadership Mission Critical Checklist © (NLMCC) to help center and guide the nurse leader’s daily work. Furthermore, the NLMCC assists busy nurse leaders to be grounded in equitable and inclusive daily work strategies. Purpose: The purpose of this innovative program is to explore the value of daily utilization of the NLMCC of staying focused on essential elements of role responsibility and the effects of use of the Nursing Leadership Mission Critical Checklist© on perceived stress, and self-esteem. Implementation: Nursing leadership students were provided information on the purpose and development of the Nursing Leadership Mission Critical Checklist© by watching a presentation, reading a book chapter and a synchronous live presentation by the authors. Students completed the perceived stress scale and self-esteem scale and were requested to use the NLMCC in their daily work for 30 consecutive working days. After the 30 days students are requested to complete the perceived stress scale and self-esteem scale, complete a questionnaire pertaining to the experience utilizing the checklist, and another synchronous live session with the authors. Results: This innovative project is currently in process and analysis of the data and lessons learned from the project will included for the final presentation 15-R. COVID-19 Pandemic and New Nurses’ Transition to Practice Outcomes: A Multi-site, Longitudinal Study Maja Djukic, PhD, RN, FAAN; UTHCS Cizik School of Nursing; Houston, Texas 10/29/2023, 11:10am - 12:00pm, Breakout: 10 he transition between nursing school and nursing practice has been well studied and recognized as a turbulent time for new nurses. Existing literature suggests that transition to practice (TTP) programs can successfully support new nurses through this challenging period. However, TTP program outcomes have not been studied related to the COVID-19 pandemic. The purpose of this study was to analyze the associations between TTP outcomes and the COVID-19 pandemic. This is a retrospective correlational, longitudinal study using secondary analysis of Vizient /AACN Nurse Residency Program survey data from the Casey-Fink Graduate Nurse Experience Survey and the Nurse Resident Progression Survey. Self-reported data from new nurses in Southeast Texas who participated in a standardized TTP program before the COVID-19 pandemic (2017–2019) were compared with self-reported data from nurses who participated in the TTP program during the pandemic (2020 and 2021). The results indicate that patient safety and commitment to staying employed in the organization and the nursing profession should be priority improvement areas for employers and TTP program staff as they work to support new nurses’ TTP in a pandemic. 16-QI. Answering the Call: Development of a PACU Nurse Residency Program Kathleen Diatta, PhD, RN, NE-BC; Emory University Hospital; Atlanta, Georgia 10/29/2023, 12:00pm - 1:50pm, Poster Session Perianesthesia leaders have long struggled to meet the staffing needs required to safely care for patients. Lack of exposure to perianesthesia-specific content in academic programs, burnout rates, excessive workloads, work-life imbalance, inefficient work processes, and nurse-physician relations have highlighted the importance for perianesthesia nurse residency programs. As contract labor nurses look to return to the workplace, perianesthesia leaders must be ready to provide an organized transfer of knowledge offered by residency programs that minimize vacancy rates, promote retention, and support staffing guidelines. The concept of nurse residency programs is not new. However, nurse residency programs in perianesthesia and procedural areas are in its infancy stages. Applying Benner’s theoretical framework to the perianesthesia nurse residency program allowed educators to plan and prepare for the competency regression that naturally occurs as nurses’ move through different clinical specialties. Researchers found that offering specialized residency programs enhances retention, allows for customization, and creates educated and well-prepared leaders at the bedside. As facilities across the country focus on recruitment and retention efforts post-pandemic, offering a perianesthesia nurse residency program is critical now more than ever. As perianesthesia leaders plan for the future, consideration for a positive practice environment that attracts and retains talent is top of the list. Researchers reported nurses who participate in residency programs are more prepared to care for today’s complex patient population. In addition, perianesthesia departments that provide nurse residency programs foster a successful transition from novice to expert clinician. Educators from a large healthcare system collaborated in the spring of 2021, to create a nurse residency program to complement formal clinical orientation. The educators created a program geared specifically to address the competency needs and education of nurses in the postanesthesia care unit. The program was based on Benner’s novice to expert theoretical framework and ASPAN’s competency-based orientation for the perianesthesia setting. In the fall of 2021, the pilot program of eight participants launched. All participants successfully completed their residency program as well as individual unit-based orientation. Participants completed a pre- and post-program self-efficacy questionnaire. The results revealed that participant’s confidence level doubled in seven of eight categories. Subsequent programs yielded similar results. Josephine Kamera, Ed.D., RN; Middle Georgia State University; Macon, Georgia 10/30/2023, 10:35am - 11:30am, Breakout: 19 International nursing students have high attrition rates in nursing school. This study was a qualitative, interpretive hermeneutic phenomenological that explored eight multinational nursing students’ experiences while enrolled in a nursing program. In-depth interviews were conducted, and three themes emerged: Barriers – related to technology, language, finances, stereotypes. Relationships – related loneliness/isolation, support, students’ social interaction. Process - related learning environment, mentoring, supporting structures from admission to completion. The study provides a voice of international nursing students and their experiences. By understanding these students' experiences and unique challenges, nursing educators may be better able to meet their educational needs and help them to succeed. 19-ASP. Sustainable Funding in Leadership Science Connie White-Williams, PhD, RN, NE-BC, FNAP, FAHA, FAAN; University of Alabama at Birmingham Hosptial; Birmingham, Alabama 10/29/2023, 2:00pm - 2:50pm, Breakout: 13 Problem/Background/Significance, Rationale: There is little information known on how to sustain innovative care delivery models to meet the needs of underserved populations within an academic health system. Leveraging the relationship of academic and practice partners as well as the alignment with health system, community partners, and funding agencies, nurse leaders have been able to sustain and grow an interprofessional collaborative practice (IPCP) model to provide equitable and inclusive care for a vulnerable heart failure population. Purpose, Specific Aims, Project Goals or Objectives: The purpose of this presentation is to describe the longitudinal approach used to sustain an interprofessional care delivery model with and without grant funding, and discuss the outcomes and lessons learned over this 9-year partnership. Included in the presentation is a discussion of how to leverage grant funding resources to address research questions in leadership science. Methods, Collaboration, Implementation and/or Evaluation Plan: Born from an initial 3-year grant funding (2014-2107), the nurse-led IPCP Heart Failure Transitional Care Services for Adults (HRTSA) Clinic was sustained by the health system to provide care to an underserved heart failure population. Underserved patients who experience the adverse effects of the downstream social determinants and have a diagnosis of heart failure are at risk for poor outcomes; thus, the clinic’s mission is to provide guideline directed medical therapy, reduce repeated hospitalizations, and reduce costs. Nursing leaders have collaborated with the health system for resources needed for daily operational needs. Funding (2018-2023) concentrating on behavioral health added additional resources for patients in need of counseling and behavioral health resources. Heart failure care in rural areas is known to be less equitable. Thus, a grant (2019-2022) was awarded focusing on ambulatory care nursing in rural areas in which students rotated clinical hours through the clinic. Sociodemographic, clinical, and financial data are collected and used to evaluate outcomes. Results/Outcomes and Implications: Through the years the clinic has been able to increase the number of unique patients and appointments over time resulting in a care delivery model that can reduce hospital readmission days by 80% and lower costs of care in underserved patients with heart failure. Overall financial cost avoidance savings was $7,459,429 in patients from 2015-2022. Dissemination of our work includes over 50 local, regional, national and international presentations as well as 18 peer-reviewed publications. The trusting and unselfish relationship of the nursing partners who employ IPCP principles may be the key to sustaining and achieving optimal clinical, financial, and quality patient outcomes. Understanding the vital role of IPCP may assist healthcare systems to implement care delivery models to achieve outcomes that provide equitable and inclusive care. Similarly, savvy in leveraging grant funding resources to address research questions in leadership science related to care delivery model design has helped to sustain the work using targeted outcome data. 20-EBP. Nursing Leadership Development: Recommendations from A Systematic Review Lozay Foots III, DNP, MS, FACHE; San Antonio, Texas 10/29/2023, 2:00pm - 2:50pm, Breakout: 15 Background: As the consistent 24-hour presence in hospitals, nurses play a pivotal role in ensuring quality and safety (Q&S) of patient care. However, a comprehensive review of evidence suggesting the most impactful recommendations to guide nursing interventions that enhance patient safety and quality care is lacking. Purpose: The purpose of this article is to describe a systematic literature review to create recommendations for developing the Q&S component of a nursing professional practice model for the U.S. military. Methods: We conducted a systematic literature review across five databases. Results: Included for review were 249 articles. From these articles, we created 94 recommendations for practice in eight focus areas: 1) Communication; 2) Adverse events; 3) Leadership; 4) Patient experience; 5) Quality improvement; 6) Safety culture/committees; 7) Staffing/workload/work environment; 8) Technology/electronic health record. Conclusion: These findings provide suggestions for implementing Q&S practices that could be adapted to any health system. Key words: quality, safety, nursing, systematic review 21-R. Examining Moral Injury, Well-being, Resilience, and their impact on Nurse Leaders' Intentions to Leave Position or Profession Amid COVID-19 Pandemic. Minjin Kim, PhD, RN; University of Cincinnati; Cincinnati, Ohio 10/28/2023, 2:10pm - 3:00pm, Breakout: 2 Background: The focus on MI among healthcare professionals, particularly nurse leaders, intensified in 2021 due to the pandemic. Limited studies have explored the association of intention to leave position with MI, well-being, and resilience, with even fewer providing implications for leadership and management. Objective: In this study, we examined variables of moral injury (MI), well-being, and resilience and associations with intention to leave position and the profession among nurse leaders during the COVID-19 pandemic. Methods: The study included 273 nurse leaders in Ohio. Analyses were conducted to identify differences in MI, well-being, and resilience based on intent to leave the current position compared to intent to leave the profession. Logistic regression models were then estimated to determine the effects of MI, well-being, and resilience on intent to leave. Results: In the study sample, 92.4% were female, 86.9% were white, and 70.5% held a baccalaureate degree or higher. The intention to leave one's position was significantly associated with moral injury (MI) and negatively associated with resilience. However, there was no association found between MI, resilience, and well-being with the intent to leave the profession. In the multivariable regression analysis, only the total well-being score showed a significant association with the intention to leave the position. Conclusion: The multivariable regression analysis identified overall well-being as the primary factor affecting nurse leaders' intention to leave their positions, highlighting the importance of healthcare organizations fostering nurse leader well-being. Additionally, the analysis showed a significant positive association between moral injury and intention to leave, indicating that addressing moral injury is crucial in reducing nurse leaders' intention to leave. Furthermore, a significant negative association between resilience and intention to leave was found, suggesting that enhancing resilience plays a vital role in promoting nurse leader retention. These findings emphasize the need for targeted efforts to create supportive environments that foster well-being, and resilience, and address moral injury in order to maintain a stable and effective nursing leadership workforce. Further investigation is needed to explore the unique challenges faced by nurse leaders from diverse backgrounds. 22-R. Incivility and the Impact of Nurse Leader Styles and Characteristics Karen Fowler, Ph.D., RN, CENP; University of Texas at El Paso; El Paso, Texas 10/28/2023, 3:10pm - 4:00pm, Breakout: 6 Incivility and the Impact of Nurse Leader Styles and Characteristics Abstract Background- Nursing professionals account for the most significant number of healthcare providers, and their ability to maintain positive relationships with healthcare provider peers and the patients they serve is crucial for safe patient care delivery. According to the Bureau of Labor Statistics, the expected growth rate from 2020 – 2030 for the Registered Nursing (RN) workforce is 9%, with a projected 194,500 openings per year. Before the COVID-19 pandemic, a forecast model projected a shortage of 510,394 RNs by 2030 (Zhang, Tai, Pforsich, & Lin, 2018). We now know this value is much more excellent with the impact of COVID on the nursing workforce and incidences of incivility. Workplace incivility that goes ignored can cause nurses to feel unvalued, which can affect team dynamics and influence the intent to leave the organization or profession. The concept of incivility in the workplace is not new to nursing. In 2004, the Institute of Medicine outlined nurse leaders' significance in the workplace environment and nursing care delivery. The concept is engrained through our personal beliefs and values in that we respectfully treat those we interact with the way we expect to be treated. Nursing leaders have a complex role in healthcare. One of many responsibilities is their critical role in advocating for patients and their team members. Objective- The study aimed to investigate the impact (or lack of) of leadership styles on the frequency of incivility. No studies could be found post-COVID on this specific topic indicating that this study has the potential to provide evidence currently lacking in the literature. Methods- A quantitative exploratory approach was used. During civility training in El Paso, Texas, the Multifactor Leadership Questionnaire (MLQ 5X) and the Workplace Incivility Survey (WICS) were administered to acute care nurses. Data analysis was conducted using descriptive statistics and multivariate correlational analysis. Results- Perceived negative leadership characteristics were significantly correlated with the incidence of incivility in the workplace. Linking Evidence to Action- Tactics and strategies must be deployed to support nurses and nursing leaders in creating a civil workplace. Close monitoring of nurse leadership characteristics will enable organizations to help and offer education/training to nurse leaders, thus influencing the incidence of incivility. Key Words- Nurse Manager, Leadership, Multifactor Leadership Questionnaire, Transformational Leadership, Transactional Leadership, Passive-Avoidant Leadership, Leadership Styles 23-QI. Empowering nurse leaders to re-think and re-engineer the practice environment through the use of a conceptual framework for nurse retention Sarah Lackey, DNP RN CMC; Cone Health; Greensboro, North Carolina 10/28/2023, 3:10pm - 4:00pm, Breakout: 4 Nurse retention is a critical issue. The literature is filled with information about strategies, approaches, initiatives, and best practices. There is often little bandwidth to peruse the literature and consider a broad range of retention strategies. To date, nurse retention has frequently been a mixture of intuition, creativity, and broad action planning. There is an absence of organizing structures to help leaders think about the issues, organize data, and engage in targeted problem solving. Additionally, the typical cadence for implementing action plans for retention includes unavoidable drift as the demand of the work necessarily overrides other processes. To create a structure that would assist nurse leaders, a conceptual framework for nurse retention was constructed using two simple theories and concepts derived from qualitative analysis of empirical outcomes for intent to stay, intent to leave, turnover and retention. A process to evaluate and address retention issues within the practice environment using the Framework was piloted; after encouraging results from the pilot study, a QI project was designed. The project involved four inpatient units. The methods for data collection, data mapping, action planning, implementation and evaluation were well defined. The process used the Framework to organize data and guide actions, and resulted in strategic, targeted work that also conserved time and resources. The planning considered individual unit culture, the nurse management team’s strengths, and insisted upon using data pulled directly from staff input. Nurse leaders extolled the simplicity and ease of use, and experienced a sense of confidence that they were addressing relevant work environment-related retention issues with a high potential for impact. Quantitative and qualitative data were collected from system dashboards and surveys. Outcomes included improvement in voluntary turnover rates in 3 of 4 units; improvement in vacancy rates in 3 of 4 units; improvement in work effectiveness scores (Laschinger’s Work Effectiveness Tool II) in 3 of 4 units, involving 4-8 nurse retention concepts. Scores that represented communication, support and recognition improved in each surveyed department. Overall employee engagement scores, part of the vendor directed survey done periodically in the organization, showed improvement. The score that showed the most improvement – rising an average of .215 and increasing in every participating unit - was the response to the question: “I would like to be working at this organization 3 years from now.” Pre implementation data for turnover by headcount were collected for six months before implementation as a baseline. During the six months of implementation, and the six months after implementation, the three successful units demonstrated a total reduction of turnover by head count that resulted in savings of $1,256,400, calculated according to NSI 2023 average cost of RN turnover. Lessons learned include the efficacy of using a conceptual framework to ensure a common language for nurse retention; the importance of applying the two theorists in decision making given limited resources of time and energy; one-up support and involvement; resisting the urge to plan actions before all data have been collected and mapped; not over-thinking the process. 24-R. Modern Perceptions of Leadership as an Influential Factor in Nursing Retention: A Phenomenological Study M'Lyn Spinks, DNS, RN, CHSE, CNE, FCN; Kennesaw State University; Kennesaw, Georgia 10/29/2023, 10:10am - 11:00am, Breakout: 9 Research on the retention of professional nurses has identified the importance of leadership systems that support nurses. However, pilot data by the lead author indicated that the burgeoning workforce of millennials and Gen. Zs does not value the characteristics modeled in existing leadership theories. In the pilot study, cognitive interviews with a sample of millennial nursing students born between 1982 and 2000 revealed that they did not recognize the identified authentic leadership behaviors as desirable, nor could they articulate awareness or appreciation for authentic leadership qualities. Thus, the research findings that identify a positive relationship between nursing retention and Authentic Leadership Theory have yet to be confirmed with populations of nurses born after the 1980s. This study aimed to understand the perceptions and experiences of nursing leadership of final-semester baccalaureate nursing students born after 1982 and before 2000. Furthermore, the researchers sought to determine if any alignment existed between the participants’ perceptions and experiences of leadership and the core traits of Authentic Leadership Theory. The specific aims of this proposed study were to: 1. Examine millennial baccalaureate nursing students’ perceptions of nursing leadership. 2. Identify similarities and dissimilarities between millennial baccalaureate nursing students’ perceptions of leadership and the four dimensions of authentic leadership theory: self-awareness, relational transparency, balanced information processing, and internalized moral perspective. Authentic Leadership Theory, because of its known relationship to nursing retention and its prevalence in nursing leadership literature, was selected as the theoretical framework for this study. The interpretive phenomenological research design was chosen to fulfill the purpose of understanding participants’ perceptions and experiences. Data were thematically coded and analyzed using interpretive phenomenological analysis (IPA). Themes were identified from participant quotes based on a combination of occurrence and richness. Richness is attributed based on the participant's depth of description and length of the quoted passage. The setting was a large, southeastern urban university, and the sample (n=16) consisted of millennial nursing students in their final semester of an accredited baccalaureate nursing program. Data were collected via audio-recorded, face-to-face interviews. The face-to-face interview was semi-structured based on an interview guide of open-ended questions, follow-up, and probing questions from a preliminary literature review. The data were de-identified, numbered to correspond with the researcher's field notes, and transcribed verbatim. Data were thematically coded and analyzed using interpretive phenomenological analysis (IPA). Themes were identified from participant quotes based on a combination of occurrence and richness. Richness is attributed based on the participant's depth of description and length of the quoted passage. Applying the process of interpretive phenomenological analysis (IPA) outlined by Smith, Flowers, and Larkin (2009), six themes and associated sub-themes were identified from the participants’ interviews: 1) nursing leadership is a position, 2) our relationship is important to me, 3) we’re all on the same team, 4) see me for who I am, 5) an effective leader is a mentor, and 6) an effective leader is a problem-solver. 25-EBP. The Hospital-Based Nurse Scientist as A Senior Nurse Leader: Evidence to Support the Role Esther Chipps, PhD, RN, NEA-BC, FAONL; The Ohio State University; Charlotte, North Carolina 10/29/2023, 2:00pm - 2:50pm, Breakout: 15 The literature addressing the role of the HBNS has grown in the past two decades. However, the literature is largely expert opinion, with some descriptive studies focusing on skills, role, and role-related outcomes. The contributions of the HBNS to the senior nursing leadership team have not been well described in the literature. Anecdotal reports indicate that the HBNS does play a significant role on the leadership team as an inspirational leader, scholar, innovator, and advisor on relevant nursing issues. Now more than ever, innovative strategies are needed to build and evolve hospital-based programs of nursing scholarship. The COVID-19 pandemic facilitated a shift in the national nursing leadership research agenda, bringing intensified attention to testing new nursing care delivery systems and addressing the social determinants of health/health equity to improve social care outcomes. To keep pace with the changing healthcare landscape, nurse leaders should consider including hospital-based nurse scientists (HBNS) on their leadership teams to influence and address the future of nursing practice. Moreover, the power of the nurse scientist and nurse leader dyad working toward addressing the Institutes of Medicine’s Quintuple Aim cannot be underestimated. The HBNS’s role is multifaceted and significantly different from a traditional academic role. Based on the current evidence and support in the literature for the HBNS role, hospitals have multiple options to develop and implement a sustainable program of clinical research under the leadership of the HBNS. 26-EBP. Leadership WalkRounds: Implementing an Evidence-based Rounds in Acute Care to Increase a Culture of Safety. Todd Tussing, DNP, RN, CENP, NEA-BC; The Ohio State University; Columbus, Ohio 10/29/2023, 12:00pm - 1:50pm, Poster Session Nurses have experience and knowledge of risks that may lead to patient harm, additionally, nurses need education to mitigate risk as well as know their resources for support when a risk for patient harm has been identified. Evidence on Leadership WalkRounds has demonstrated that they are effective in increasing staff perception of a culture of safety, staff well-being, and decrease staff burnout. The current work environment within nursing units has changed in the last several years since the onset of the Coronavirus pandemic. Currently, nurses are not only resigning from inpatient nursing positions, but leaving the profession citing negative work environments and the impact of the current nursing shortage. Leadership WalkRounds offer an intervention that can be utilized in today’s chaotic and stressful healthcare environment. To identify risk concerns and to educate nurses on the management of risk, Leadership WalkRounds were implemented at two hospitals which are part of an academic medical center. The joint rounds were comprised of nursing administration from the hospital, a nurse attorney, and nurse/paralegal from the Risk Management/Legal Affairs Department of the medical center. Leadership WalkRounds involving a nursing director from the hospital, nurse attorney, and nurse/paralegal from the Risk Management Department were conducted on inpatient nursing units, emergency departments, one procedure unit, and an outpatient clinic spanning multiple days and including the night shift. Rounds occurred over a 6-week period. Nurses were encouraged to talk to the joint leadership team and was provided a survey to elicit their suggestions for risk mitigation education. Three sets of joint rounding were completed over a 6-week period involving both day and night shifts. Two hospitals were the setting for the rounds (one academic, the other urban, community) involving 7 medical-surgical floors, 1 ICU, one ICU Step-down, 2 emergency departments, one endoscopy unit and one outpatient wound care clinic. Over 300 patient care staff participated in the rounds. 157 surveys were returned (117 RN/APRN; 40 other). Issues identified: care coordination in the perioperative department, patients who leave the nursing unit unaccompanied, violence from family/visitors, and family/visitor recording care with mobile devices. Based on the rounding feedback, two separate sets of rounds were implemented in which the team collaborated with the leadership of Safety and Security to address staff questions/concerns regarding patients leaving the unit and family/visitor violence. 27-EBP. Strategic Planning: Moving from Plan to Implementation Teresa Welch, EdD, MSN, RN, NEA-BC; The University of Alabama; Tuscaloosa, Alabama 10/29/2023, 12:00pm - 1:50pm, Poster Session Rationale. Successful organizations depend on strategic thinkers and decision-makers who understand strategic planning and strategic management. These strategic leaders can proactively manage the constant environmental change to position their organizations for a competitive advantage and avoid acting in a reactive and defensive manner. However, while organizations are often adept at developing detailed and extensive strategic plans, implementation of the plan is often poorly implemented or without a definitive strategy. The aim of this presentation is to address key strategies for successful implementation of the strategic plan to support strategic decision-making, bring about sustainable cultural change in an organization, and meet the organization’s overall strategic goals using the principles of implementation science as a framework for change. Implications for nurse leaders. Nurse leaders are uniquely positioned within the organization to recognize the need for change and the necessary resources to not only implement but sustain change over time. They are the perfect champions for leading the implementation of evidence-based practice projects in hospitals and healthcare systems. Tenets of evidence-based practice are now embedded into many facets of nursing education and directly incorporated into American Association of Colleges of Nursing’s (AACN’s) Nurse Essentials’ curriculum guidelines. However, while often one thinks of evidence-based practice somewhat in isolation, the field of implementation science provides both broad guidelines and specific models to advance EBP directly into implementation plans to create sustainability. Implementation science also promotes evaluation plans to help determine the success of a project, and to facilitate dissemination of project results. While strategic planning is a key component of an organization’s long-term viability and strength, implementing projects successfully is imperative. Through the field of implementation science, leaders can draw strategies and specific models to guide their implementation plans and successfully lead their organizations. Relevance to Theme: Strategic planning, strategic decision-making, and strategic management are directly correlated to an organization’s ability to implement sustainable initiatives to change organizational culture when building healthy workplaces that provide the infrastructure to support an equitable and inclusive future for all stakeholders. 28-EBP. Cultural Intelligence: Honoring the Shared Human Experience Through Human-Centered Leadership Lucy Leclerc, PhD, RN, NPD-BC; uLeadership; Atlanta, Georgia 10/28/2023, 3:10pm - 4:00pm, Breakout: 4 While the ground continues to shift beneath our healthcare feet during global challenges from political unrest to war to the persistent peripandemic world we now live in, the shared human experience is a common denominator. As healthcare leaders, providers, and community advocates, there must be a way to honor and celebrate differences alongside similarities in the diverse and beautiful interactions we have each day with diverse and beautiful humans. Human-Centered Leadership in Healthcare (HCL-HC), a contemporary, evidence-based, relational leadership theory, was used in a leadership development series with nurse leaders from across the globe as a lens to view and address variables related to justice, equity, diversity, equality, and belonging. Principles of Cultural Intelligence (CQ) provided a common language and shared vision to guide leaders in how to value, honor, and navigate differences in their teams, colleagues, patients, and communities. Four nurse leader cohorts were grouped according to emerging and experienced leaders with 40 nurses per cohort. The series was delivered virtually and synchronously with participants from Asia, Africa, and the United States. Principles of CQ including Cognition, Megacognition, Motivation, and Behavior were aligned with an active learning process embedded in the HCL-HC theoretical model of Self, Awakener, Connector, and Upholder. The leaders engaged in dynamic learning through exposure to CQ and HCL-HC followed by activation of the material through CQ self-assessment and designing an action-oriented plan to strengthen CQ. Thematic analysis of evaluations and feedback revealed an interesting, common realization that HCL-HC and CQ provide a practical lens through which leaders are better equipped to honor the shared human experience of staff, colleagues, patients, families, and communities. 30-R. Leveraging Social Media to Create an Equitable and Inclusive Future for the Nursing Workforce Heather Nelson-Brantley, PhD, RN, NEA-BC; University of Kansas; Kansas City, Kansas 10/29/2023, 3:00pm - 3:50pm, Breakout: 17 The use of social media has grown exponentially over the past decade, with approximately 72% of Americans reporting they use some type of social media as part of their daily activities. Facebook, Instagram, Twitter, reddit, LinkedIn, YouTube, and other social media platforms have become important avenues for not only sharing information but also powerful tools for connecting, building relationships, and influencing thought. Like all of society, nurses use social media, making it a particularly important avenue for connecting, attracting, and retaining a diverse and inclusive nursing workforce. Yet, nurse leaders express having minimal experience with effectively using social media to influence the profession. Because of this, nurse leaders miss critical opportunities to connect, attract, and retain nurses and advance nursing leadership research, education, practice, and policy. Our review of the literature identified no studies that comprehensively examined nurses’ use of social media, how their use varies by different demographics, and how these factors inform their decisions about current and future employment. Nurse scientists from the ALSN research committee are conducting a 3-phase study, guided by the Social Media Engagement framework, to examine nurses’ use of social media and how it impacts their job decision-making. This presentation will focus on Phase 1. The overall objective of Phase 1 is to describe: (a) nurses’ use of social media for professional purposes, and (b) the association between nurse characteristics (e.g., age, race, ethnicity, gender identity, sexuality, geographic location, veteran status, ability, years as RN/APRN, education, certification type of nursing) and social media use for job decision-making (e.g., contemplating leaving/staying in their current position, looking for new opportunities, etc.). This study uses a cross-sectional, quantitative descriptive survey design. The setting and sample include registered nurses and advanced practice nurses currently working in the U.S. in any setting (e.g., acute care, ambulatory care, education, research, policy), that have at least one month of nursing practice, and use social media. Participants were recruited through AMN Healthcare’s database of over 1.4 million nurses, the Versant database, ALSN, and social media influencer posts. A 28-item survey was developed by the research team and informed by a review of the literature. The survey includes demographic questions, as well as questions about their use of social media and their current employment. Descriptive statistics and correlational analysis were used to analyze the data. Results will be shared during the presentation. This study helps fill an important gap in the literature by identifying social media platforms that nurses use and how they use them for making job-related decisions. Additionally, we describe the relationships between social media use, nurse characteristics, and job decision-making. This study advances nursing leadership research, education, and practice by enhancing the ability of nurse leaders to connect, attract and retain nurses; thus, adding a much-needed approach to the multifaceted solutions for addressing the critical nursing workforce shortage and building an equitable and inclusive future. 31-ASP. Clinical Scholars Program: Building leadership capacity through an academic-clinical partnership Tedra Smith, DNP, CRNP, CPNP-PC, CNE, CHSE; University of Alabama at Birmingham; Birmingham, Alabama 10/29/2023, 12:00pm - 1:50pm, Poster Session Background: Quality improvement (QI) initiatives in pediatric healthcare settings have increased over recent years; however, gaps remain between the care provided and what the evidence states is best practice. Although most pediatric care is provided by nurses, nurses often report a lack of preparedness and resources to engage in evidence-based practice (EBP) and QI initiatives needed to advance best practice standards. Children’s of Alabama (COA) is the only free-standing healthcare facility in Alabama focused on comprehensive care for children. COA employs approximately 2,036 nurses. Nurses are hired from various educational backgrounds, clinical expertise, and leadership experiences. Most nurses lack formalized leadership development to build the knowledge and skills necessary to lead teams, guide, develop, and implement plans for quality improvement work. In 2013, COA partnered with the University of Alabama at Birmingham School of Nursing (UABSON) to develop the Jarman Lowder Clinical Scholars Program. Leadership within COA and UABSON recognizes the need to expand the program to include leadership development and enhancement. In 2022, academic experts and COA nursing leadership expanded the program to include leadership knowledge and skills in parallel to the QI content in place. This is timely as the Future of Nursing 2020-2030 Report directly addresses the need to expand the number of nurses in leadership roles. Purpose: The purpose of this program is to provide an experiential learning opportunity for future nursing scholars in leadership and quality improvement. The program facilities professional leadership development among COA staff nurses for potential advancement and leadership opportunities. Participants engage in activities to strengthen communication, identify gaps in healthcare processes, and lead healthcare improvement initiatives. Collaboration and Evaluation: Program faculty collaborated with COA nursing leadership to identify development needs for leadership and quality improvement. Program faculty appraised literature to design a 12-month program for sequential knowledge and skill advancement. Each session contains a didactic content review with open discussion of case studies and scenarios. The scholars then apply this knowledge and skills in subgroups through simulation, case study discussion, and reflection. Participants identify a gap in clinical practice, gather supportive internal and external data, ideate a change or improvement, and prepare to launch the quality improvement project. Included in the program is personal reflections, emotional intelligence, crucial conversations about sensitive issues, leading teams, scholarly dissemination through public speaking, participation in COA Governance activities, and innovations in healthcare improvement. Engage in coaching participants in presentation creation, development and publication of scholarly work, CV/resume development, and career planning. Outcomes and Implications: Participant feedback from inception indicates the program is an effective method of knowledge development and skill application. The program has been successful with increased numbers of participants year after year. Fifty scholars have successfully completed the clinical scholars program. Project outcomes have included increased communication between nurses and families with the implementation of a standardized transfer protocol, reduction in return emergency department visits for fever with the implementation of a fever education handout, and improved utilization of resources with the implementation of focused discussions on resources with the nursing staff. 32-QI. Cultivating Organizational Change Toward Cultural Awareness in Nurses Through Continued Education Kemi Reeves, MSN, RN, GNP-BC; UCLA Health; Los Angeles, California 10/29/2023, 12:00pm - 1:50pm, Poster Session Background: The foundational aspects of racism in American society are embedded within educational and health systems, the central institutions where nurses train and work. Racism in nursing is displayed within American nursing institutions. Once minority nurses enter the job market, they risk being exposed to overt acts of racism and microaggressions from patients, peers, and supervisors (Tobbell & D'Antonio, 2022). In 2021, the American Nurses Association created a National Commission to Address Racism in Nursing that surveyed nurses nationwide. From this nationwide survey, the commission found that most nurses surveyed shared that they have personally experienced racism in the workplace, with the transgressors being a peer, patients, managers, or supervisors (Tobbell & D'Antonio, 2022). Purpose: The purpose of this quality improvement project is to determine whether a 12-week evidence-based experiential nursing-centered equity, diversity, and inclusion training for in-patient nurse leaders on a unit specializing in the geriatric psychiatry improves the cultural awareness and responsiveness of nurse leaders. Methods: This project will utilize a pre-test and post-test intervention design. The setting for this project will be a large academic health system in southern California; more specifically on an in-patient geri-psychiatry unit. This project will use a convenience sample of nursing staff in leadership roles in the in-patient geri-psychiatry unit. The project will occur over 12 weeks by a review of the Safely Opportunities for Improvement (SOFI) event reporting system, a review of health system policies that address discrimination, and implementing a case-based nursing education program training offered by the American Nurses Association, National Commission’s Project ECHO® on Racism in Nursing. Data Collection: The Nurse Staff Cultural Awareness Scale will be administered pre-intervention and post-intervention to analyze the mean difference in the pre-intervention and post-intervention cultural awareness results. Policy adherence will be assessed by measuring SOFI report volume from the unit where the project will be implemented. A raw number and percentage change in report volume will be calculated. Descriptive statistics will be used to analyze the change in report volume pre-intervention and post-intervention. Feasibility will be assessed based on the dropout rate, attendance rate, average completion rate, and the post-intervention feasibility survey. Descriptive statistics will be used to analyze feasibility metrics. Implications and Potential Benefits: The benefit for participants is the potential to improve adherence to the health system policies, offer greater skill and confidence when addressing incidents of discrimination on the unit. Participants may leave the project with improved awareness and knowledge about racism in nursing, and cultural self-awareness. Although the education series targets the collegial interactions of the nursing profession, the education and skills translate nursing practice, patient care, and have the potential to improve patient outcomes. Fostering a culture of equity, diversity, and inclusion has been shown to led to a decline in incivility, lateral violence, and harassment, thus promoting a culture of care, wellness, and increasing quality of life (Morrison, et al. 2021). If successful, this pilot may influence future educational undertakings throughout the health system. 33-R. The COVID-19 Pandemic: Exploration of Nurse Leaders’ Experiences Managing the Clinical Environment during a Crisis Chika Anueyiagu, DNP,RN, FNP, NE-BC; Yale New Haven Health; new haven, Connecticut 10/29/2023, 11:10am - 12:00pm, Breakout: 12 The COVID-19 Pandemic: Exploration of Nurse Leaders’ Experiences Managing the Clinical Environment during a Crisis Problem/Purpose The COVID-19 pandemic created novel nursing management challenges and opportunities. Nurse leaders’ roles and responsibilities needed to shift rapidly to integrate several core competences of effective crisis leadership. This study examined the experiences of nurse leaders managing setting during the COVID-19 pandemic. Objectives Three study aims included: (1) Examine leaders’ experiences during the pandemic and associated intensity of distress; (2) Describe leaders’ perceptions regarding importance and challenge associated with competencies and (3) Identify factors independently associated with leader competencies perceived as extremely challenging. Design and Methods The American Organization for Nursing Leadership (AONL) Nurse Leader Competencies served as the framework for this descriptive, cross-sectional survey-based study conducted within inpatient and outpatient settings located across a large health care system in the northeast. A previous study (Schechter, 2020) guided question selection for aim 1. The development of questions for aim 2 included a evidence synthesis integrated with AONL competencies followed by establishing content validity. Recruitment for the electronic survey targeted nurse managers began in March 2020. Randomization guided which participants received invitations at the onset of recruitment. Participants received an email invitation with link to the survey that included study information and consent. Analysis included descriptive, bivariate and multivariate testing using SPSS. Results and Conclusions. 48% (n = 151) of eligible nurse managers completed the survey. “Managing changes to unit staffing patterns” received the highest distress rating, on a scale of 1-10. The level of perceived challenge ranged from moderate to extreme. Greater than 80% rated “Managing scarce human resources” and “Making decisions without have specific details and in the absence of complete information” as most challenging. Aim 3 analysis intends to identify demographic characteristics independently associated with competencies perceived as extremely challenging; results anticipated May 2023 Implications for practice and research. Nurse leaders are pivotal for creating an optimal environment and ensuring the success of any healthcare organization. The results of this study will inform future interventions to assist clinical nurse leaders in supporting the emotional needs of staff, prioritize strategies to stabilize, increase and retain the workforce. Study results leads to opportunities to innovate and reimagine programs that are equitable and inclusive where diverse leaders can thrive and successfully lead through crisis, ambiguity, and chaos. Additionally, the opportunity is presented to advance the science of nursing leadership. 34-QI. Are We Measuring Our EDI performance? That is the Question for "U"CLA Kemi Reeves, MSN, RN, GNP-BC; UCLA Health; Los Angeles, California 10/28/2023, 3:10pm - 4:00pm, Breakout: 5 Background: A 1998 committee assembled by the Institute of Medicine highlighted the importance of health determinants and health outcomes as indictors requiring the attention of health care providers (Morrison, et al., 2021). University of California Los Angeles Health (UCLA Health) acknowledges the existing health disparities within healthcare and understands the importance of creating an institutional culture rich in the principles of EDI and their impact on the work environment, patient outcomes, and organizational performance. The collection of EDI performance measures approaches healthcare equity, modeling the process taken to assess other crucial patient safety priorities. EDI performance measures provide institutional leaders with the necessary information to optimize performance to foster sustained efforts toward advancing health equity, diversity, and inclusion. Problem: The lack of standard metrics assessing EDI performance across the nine service line of UCLA Health. Purpose: Council members identified the need for standard metrics assessing EDI performance across the nine service lines of UCLA Health. The purpose of the quality improvement project is to create and implement standardized EDI Press Ganey (PG) questions to be included in PG survey across the nine service lines. Method: The Unity in Diversity Council (UID) used the Plan Do Check Act process as a model for designing the quality improvement. Plan: UID members identified the need for standard metrics assessing EDI performance across the nine service lines of UCLA Health. Do: UID began the process by reviewing the PG questionnaires across all service lines assessing if EDI performance was measured and if there are specialty-specific EDI measures are appropriate. UID determined the need for standardized EDI questions, as it allows for an internal comparison of EDI performance. UID developed standardized EDI questions to be applied to all service line questionnaires. Check: Service line directors reviewed the proposed EDI questions and suggested edits were considered and incorporated if appropriate. The service line directors, the Chief Nurse Executive Council (CNEC), and the Office of Health Equity Diversity and Inclusion (Office-HEDI) approved the revised questions. Act: Once approved, the questions were included in the UCLA Health PG questionnaires. Outcomes: After the EDI questions were included in the PG questionnaires, there were concerns about the questions' literacy and readability level and if EDI-specific comments would appear in the overall assessment comment section. UID approached PG to optimize the literacy and readability level of the questions. After optimization, the questions were again revised to avoid linking gender identity and sexual orientation. UID requested approval from the Office of Patient Experience regarding the language of the updated questions: 1) During your stay, how well did the staff respect your cultural, racial/ethnic, religious needs and preferences? 2) If you do not speak English at home, how well did we communicate with you? 3) During your stay, how well did the staff respect your gender identity? Currently, we are waiting for guidance on the optimized language, then will request final approval to update the EDI PG questions from the CNEC, the Office-HEDI, and the Hospital Executive Leadership Meeting. 35-EBP. Expanding Stakeholder Access, While Protecting Your Intellectual Property Rights: Developing and Disseminating Evidence-Based Resources to Support Leadership Practice. Joy Parchment, PhD, RN, NEA-BC, CPDC; University of Central Florida; Orlando, Florida 10/29/2023, 12:00pm - 1:50pm, Poster Session Nurse managers, and those serving in interim nursing leadership roles, often assume their roles with little to no preparation. Increased complexity in the nurse manager practice environment warrants the rebuilding of the front-line nurse leader role. Though a plethora of evidence exists about nurse manager practice, relevant, usable, and accessible resources that can expand the leadership capacity of the interim nurse manager are not currently available. Additionally, while new nursing leadership knowledge continues to be generated, the uptake of that knowledge into professional nursing practice lags behind, failing to benefit the intended frontline nurse leader in a much needed and timely manner. Informed by research evidence, nurse researchers moved beyond traditional dissemination methods and developed an evidence-based resource for the interim nurse manager. To facilitate access to the developed resource by the intended target audience, researchers identified and collaborated with relevant stakeholders to determine the best electronic platform that could facilitate accessibility and allow for tracking its use. In addition to collaboration with stakeholders, nurse researchers engaged technology transfer experts to ensure intellectual property protection of the developed product. The rebuilding of nurse leaders cannot fully take place without open and available resources to support leadership practice now and in the future. 36-QI. Improving outcomes for advanced heart failure patients using a nurse-lead quality improvement program in Brazil Marluci Andrade Conceição Stipp, Full Professor; Universidade Federal do Rio de Janeiro; Rio de Janeiro, Brazil 10/30/2023, 10:35am - 11:30am, Breakout: 20 Background: Despite the optimization of clinical and pharmacological treatment, patients with heart failure (HF) may present refractoriness and disease progression, increased limiting symptoms and re-hospitalizations, making patients’ care increasingly complex and demanding, including in Brazil. Nursing leadership is at the core of optimizing care within institutions, utilizing and adopting new technologies, and improving care process that can provide personalized and safe care. For this, it is necessary to specialize and increase the workforce to guarantee the quality of the care process. Objective: To describe the implementation of a nurse-lead advanced heart failure management program to improve the use of evidence in the care practice Method: The Knowledge to Action Framework (KTA) method1 was used in a hospital in Rio de Janeiro for a Quality Improvement project since 2012. The KTA framework was sustained in two phases: (1) the creation of knowledge-raising and synthesizing the knowledge about the care already instituted for patients with advanced heart failure, for the development of tools for to be applied in the line of transplant care and circulatory assistance, attracted to the nurse. (2) action cycle - identify, review, adapt, assess barriers, implement prevention, and monitor results in developing actions/care that occurred in the first phase. Based on the KTA framework, standard operating procedures were created by vad coordinator nurse (tools and checklist) to monitor patients in the transplant program and circulatory assistance in the pre, per, postoperative, and outpatient follow-up phases and in transitional care. Concerning circulatory assistance, training the coordinating nurse in international reference centers was necessary to improve leadership and follow-up practices in this context. The documents respected the particularities of each therapy (heart transplantation and circulatory assistance) and were stored in the updated electronic document manager, as recommended by the international certifying agency. Results: Thirty-five patients were followed up; 15 long-term support implants and 20 transplants were performed. About 20% of patients were admitted for double transplantation (heart and kidney), 20% were transplanted using temporary mechanical support, and 25% were transplanted using long-term mechanical support. Considering clinical deaths, the mean time of life in the sample of patients on circulatory assistance was 4.25 years; 50% of the patients had been using it for more than six years with long-term circulatory support therapy; in addition, the survival curve in heart transplantation in the first five years was 62.0% and in 10 years, 56.45%. The leadership of the coordinating nurse in this center of advanced cardiac inheritance allows the continuity of patient care, with the maintenance of clinical cases similar to international reference centers. Relevance to the topic: The use of KTA in cardiovascular nursing care, especially in the cardiac approach, provides rights for nurses to position themselves as leaders in the elaboration and development of safe, attractive, and equitable work processes for the local reality. Learning objectives: Evaluate the management of work processes for nursing care in advanced heart failure; Evaluate sustainable care and inclusive models of care based on the translation of knowledge. 37-R. COVID-19 Pandemic Response Implementation and the Impact on the Work Environments of Brazilian Intensive Care Units Liana Amorim Correa Trotte, Assistant Professor; Universidade Federal do Rio de Janeiro; Rio de Janeiro, Brazil 10/29/2023, 12:00pm - 1:50pm, Poster Session Problem: In Brazil, the Covid-19 pandemic created more hospital beds, especially in intensive care. Many nursing professionals transitioned their practice to cover the increased demand for care with minimal preparation. We emphasize that in places where professional training is allied to care, this challenge has become more complex due to existing social responsibility, requiring active, participatory nursing leaders more concerned with minimally sustainable work environments. Objective: To evaluate the work environment of the nursing team in intensive care units for Covid-19 in ten university hospitals in Brazil. Methods: A prospective cross-sectional study involving multicenter research was conducted. Nurses and nursing technicians were the participants in data collection. The Portuguese translation of the “Nursing Work Index Practice Environment Scale” was the study’s instrument. Data were collected between April and December 2021. Results: The sample had 431 nursing professionals, 194 (45%) nurses, and 237 (55%) nursing technicians. The average age was 41 years old, and 78% were women. The instrument’s internal consistency was reflected in a Cronbach’s alpha of 0.943. In four of the five domains, nursing technicians better evaluated the professional practice environment, and in one domain, there was no statistical difference. The professional practice environment was considered adequate, with a total average score above 2.5, even when evaluated by subscales. Furthermore, the best evaluations attributed by the participants to the PES-NWI items were related to the presence of clinically competent nurses, prescription of updated nursing care plans, relational work skills among multidisciplinary teams, and counting on the fact of managers in the units to support the activities. Relevance to the Theme: The findings suggest that nursing leaders in professional training contributed to the good results, consolidating the recognition and commitment expected from these actors in these areas of activity. Research with a qualitative approach will be necessary for a better understanding of the intrinsic factors associated with the sound findings of this study to help in the constant evolution of the formation of new leaders in similar situations. Learning objectives: To contribute to performing positive nursing practice environments can significantly improve patient care, nursing staff satisfaction, and overall health outcomes; To evaluate effective nursing coordination and leadership to sustain a healthy work environment, especially when faced with challenging circumstances and resource constraints 38-R. Mapping of terminal hygiene of intensive care beds using Lean Healthcare tools Marluci Andrade Conceição Stipp, Full Professor; Universidade Federal do Rio de Janeiro; Rio de Janeiro, Brazil 10/29/2023, 12:00pm - 1:50pm, Poster Session Introduction: Contaminated surfaces can serve as a reservoir for pathogens for long periods, making the hospital environment, even indirectly, pose a substantial risk to the patient. Currently, it is common to come across inadequate quality of care management processes, especially those that permeate the hygiene of the hospital environment. In this context, the use of cleaning and disinfection (LD) management methods is recommended as an essential part of the institutional hospital infection control program. This management is the main tool that nurses have to ensure a safe environment. Objective: To identify and analyze problems related to the terminal cleaning process (HT) of intensive care beds through Lean Healthcare tools for future improvements. Method: Observational study. Data collection took place from July 2021 to January 2022. The DMAIC method (Werkema, 2012) was used as a guide for this research, focusing on the DMA steps. Data collection took place at the Intensive Care Center (ICU) of a university hospital in Rio de Janeiro. The following tools were used: Gemba, Value Stream Mapping (VSM) and an adapted Spaghetti Diagram (DEA) to raise the problems. To analyze them and propose improvements, the Current Reality Tree (ARA) was used, the severity/urgency/trend matrices (GUT), prioritization and then the action plan (5W2H). There were on-site observations of 4 terminal cleanings and interviews with 5 service professionals. Fluorescent markers (MF) were used on heavily touched surfaces. Their residue was evaluated, serving as process quality indicators. Miro® software, Excel® and a projected physical plan of the area were used for data display and analysis. The SQUIRE 2.0 guidelines were followed through the use of Lean tools. Results: In the VSM, DEA and Gemba tools, inappropriate use of disinfectant and Personal Protective Equipment and incorrect handling of sharps were verified. The order, technique and LD movements did not conform. Some surfaces were not sanitized, while others were cleaned more than once, characterizing rework. The minimum and maximum time interval from the beginning to the end of the process ranged from 22 to 56 minutes. The percentage of complete/correct indicator of the HT process was 70%. Furthermore, the MF test demonstrated only 33% cleaning compliance. In the ARA, 5 roots causes were obtained. The lack of guidance (step-by-step) for the professional about the LD process and the absence of regular or admission training were classified by the GUT matrix as intervention priorities. Relevance to the Theme: There was no pattern in any observed TH. A lack of knowledge of the process by the executing professionals was noticed, as well as the need to implement a quality indicator for cleaning hospital surfaces. Therefore, the results summarized in this study demonstrated that the use of Lean tools contributed to managerial activities, ensuring a safe environment, possibilities for development and new reflections for the area of hospital hygiene. Learning objectives: To create of a Cleaning quality indicator; To map of the technique and direction of movements on different surfaces; To estabilish a percentage of completely and correctly cleaned surfaces. 39-R. Nurse Faculty Perceptions of Leadership Behaviors that Impact Job Satisfaction: Creating an Equitable and Inclusive Nurse Faculty Future Cori Heier, MSN, RN, CNE, CHSE, CNRN; South Dakota State University; Sioux Falls, South Dakota 10/29/2023, 11:10am - 12:00pm, Breakout: 11 Background: The United States has been experiencing a nursing workforce shortage, which was heighted as a result of Covid-19. Part of the solution to resolving the nursing workforce shortage is to produce more nurses, but unfortunately, the answer is not that simple due to the nurse faculty shortage. Nurse faculty vacancies are a persistent and growing problem. Poor nurse faculty job satisfaction is one contributor to the nurse faculty shortage. Effective leadership has been shown to improve job satisfaction. While it is known that leadership impacts job satisfaction, little is known about specific actionable behaviors academic nurse leaders can implement to improve nurse faculty job satisfaction. Purpose: The purpose of this study is to identify specific actionable behaviors that academic leaders can implement to contribute to improving job satisfaction among nurse faculty. Methods: A qualitative descriptive study informed by findings from a concept analysis of nurse faculty job satisfaction will be used to gain understanding of academic leader behaviors that impact nurse faculty job satisfaction. Semi-structured interviews with nurse faculty in the United States will be conducted. Recruitment methods include direct email, various nursing association listservs, a private Facebook page for nurse faculty, and snowball sampling. Thematic analysis with an inductive approach will be used to analyze interviews and inform data interpretation. Results & Implications: Data collection is underway, and results will be shared during the presentation. The rationale for this study is to address an important gap in understanding specific actionable behaviors that academic leaders can do to contribute to improving job satisfaction among nurse faculty. Findings from this study will be used to create an action guide for academic nurse leaders to use to improve nurse faculty job satisfaction. This action guide will assist academic nurse leaders in creating work environments that are conducive to improving nurse faculty job satisfaction and fostering an inclusive work environment. Improving nurse faculty job satisfaction is important for ensuring nurse faculty retention, and ultimately the ability to educate more nurses. 40-QI. Oral Health: Addressing Equity and Inclusion to Evade Variations in Patient Care Anila Ladak, DNP, RN, CNS, GNP-BC; UCLA; Los Angeles, California 10/29/2023, 12:00pm - 1:50pm, Poster Session In 2017, the wellness bundle initiative was developed by the chief nursing executive for a large teaching health system, which serve diverse population in Los Angeles. The five pillars of this initiative include general and oral hygiene, mobility, nutrition, sleep, and comfort. The general and oral hygiene pillar conducted a gap analysis across the health system with the school of dentistry and oral hygiene products representative. This analysis revealed variations in current products and inconsistencies in practices among specialty populations. Staff verbalized the lack of patient satisfaction with the currently available product in the organization. The overall purpose of this oral care initiative is to improve hygiene practices for all patient care populations; optimize the current products; reduce financial burden through wastage; standardize products; and enhance patient and staff satisfaction. The project was implemented by a group of key stakeholders which included dentist, dental hygienists, Advance Practice Nurses, and bedside nurses. The collaboration took place in the monthly meetings of the Wellness Council and the Nursing Evidence-Based practice council. A baseline assessment was conducted which included a survey for all frontline staff, rounding on specialty units, metrics, and review of documentation/EHR. The eLearning module was designed and assigned for required staff education in April 2023. A tool was created to include best practices for ease of staff reference and embedded in eLearning module and posted in internal website for easy access. Oral assessment documentation was optimized in EHR. Inpatient resources were identified and made available for staff. Patient/family education was reinforced to staff. The team collaborated with health system products committee to trial and implement new products and negotiate pricing. Also, streamlined the current products to reduce wastage and save financial resources. A dashboard was created with analysts and implemented to track utilization of products, and hygiene compliance metrics. The project is being evaluated based on the completion of the eLearning module, oral hygiene metrics, and financial impact. The baseline overall oral hygiene compliance was 70% in 2019, this will be compared with oral hygiene compliance in 2023. The eLearning is currently being completed by staff. The streamlining of oral care products has savings of $72K annually. The future implications include measuring patient and staff satisfaction and rounding on units to evaluate the impact of the project and potential opportunities to enhance patient care and staff satisfaction. 41-R. What Happens to Professional Identity When Transitioning from Direct Care To Leadership Roles Nelda Godfrey, PhD, ACNS-BC, FAAN, ANEF; University of Kansas School of Nursing; Kansas City, KS, Kansas 10/29/2023, 12:00pm - 1:50pm, Poster Session In this study, we explored nurse leaders’ experiences regarding how their sense of professional identity changed—and how it stayed the same—when moving from the direct care role to leading others. Four themes emerged: (1) One’s Sense of Professional Identity Is Foundational; (2) Professional Identity and Functional Role Work in Tandem; (3) Leading Expands One’s View; (4) We Must Build Bridges. Participants’ responses revealed that one’s professional identity is both dynamic and foundational and endures as an important component of one’s professional nursing life. 42-R. Relational Leadership Practices Improve Care and Nurse Satisfaction: A Scoping Review K. David Bailey, PhD, MBA, RN, CCRN-K, NEA-BC, FACHE, FAAN; UCLA Health - Santa Monica Medical Center; Santa Monica, California 10/29/2023, 12:00pm - 1:50pm, Poster Session Relational Leadership practices make a difference. Evidence identified in the scoping reviews reveals that nurse leaders who use relational leadership styles improve patient and nurse outcomes. 43-EBP. Building capacity for mentoring through educating nurse leaders Annette Harrilson, RN, MSN, DNP; Piedmont Fayette Hospital; Fayetteville, Georgia 10/29/2023, 12:00pm - 1:50pm, Poster Session Research has demonstrated a positive correlation between nurse mentoring and organizational outcomes. This project aimed to determine if an educational intervention focused on mentoring and the benefits of mentoring increased knowledge and awareness among nurse leaders at a southeastern community hospital. Seventy-two (N = 72) nurses were recruited and agreed to participate in the intervention. Ninety-three percent of the participants (n = 67) were female with the average age of the participants being 45 years (SD = 11.61). The participants had 17.25 (SD = 11.51) years of experience in nursing and were employed in their current position on average for 5.93 (SD = 6.52) years. The average pretest score was 78.19 (SD = 12.48), and the average posttest score was 83.47 (SD = 9.22). Using a paired t test to estimate the data, the correlation between the two scores was statistically significant (r = 0.41, p < 0.001), and there was a statistically significant difference in pretest and posttest scores (t = -3.70, p < 0.001), indicating an increase in knowledge. Participants were also asked to rate their awareness of nurse mentoring on a Likert scale of 1 to 7, with 1 = no awareness and 7 = full awareness. The average pretest score of awareness of nurse mentoring was 4.82 (SD = 1.46), and the average posttest score was 6.47 (SD = 0.71). Like knowledge scores, the correlation between the two scores was statistically significant (r = 0.41, p < 0.001), and there was a statistically significant difference in scores (t = -10.51, p < 0.001), indicating an increased awareness of nurse mentoring. This project contributes to positive social change as well as increasing inclusion by increasing knowledge and awareness of nurse mentoring among nurses, which can lead to improved patient and organizational outcomes. The educational intervention closed the gap in the practice problem by increasing the knowledge and awareness of mentoring and the benefits of mentoring among the nurse leaders who participated. Through the increased knowledge and support for mentoring, future mentoring programs will be developed and led by nurse leaders. 44-R. Generation Z nurses bring a new generation of diversity and passion to nursing! Margot (Lisa) Hedenstrom, PhD, RN, MSN, MBA, NEA-BC; Kennesaw State University; Kennesaw, Georgia 10/29/2023, 10:10am - 11:00am, Breakout: 9 on the healthcare industry. The literature review revealed that Gen Z nurses bring several unique attributes to the profession, such as being skilled in the use of technology, having a strong desire for work-life balance, and valuing diversity and inclusion. Additionally, they have a strong sense of purpose and are driven by a desire to make a difference in their profession. These characteristics are becoming increasingly important in the healthcare industry, as it faces new challenges such as the aging population, the increasing demand for healthcare services, and the need for innovative solutions. Gen Z nurses are well-positioned to address these challenges, using their technological skills, their commitment to work-life balance, and their desire to make a positive impact. Overall, understanding the common characteristics and learning needs of Gen Z nurses is crucial for developing effective strategies to support and retain them in the nursing workforce. The identified practices, such as providing opportunities for professional development, promoting work-life balance, incorporating technology in education and training, and fostering a culture of inclusivity and diversity, can be useful for organizations to attract and retain Gen Z nurses and ensure the continued provision of high-quality nursing care. In terms of practice recommendations, it is important to understand the learning styles of Gen Z nurses and how common characteristics impact their transition to practice. By understanding their preferences for experiential and collaborative learning, technology usage, and feedback, nursing education programs and onboarding processes can be modified to better meet their needs. Additionally, there may be a need for mentorship programs, leadership development opportunities, and support networks to help Gen Z nurses navigate the transition to practice successfully. This information can assist the nurse leader who is managing a multigenerational workforce. In summary, further research is needed to understand the needs and learning styles of nursing students and practicing nurses, particularly Gen Z nurses, and how these can be effectively incorporated into nursing education and onboarding processes. By implementing appropriate changes, nursing educators and healthcare organizations can better engage and support the next generation of nurses, ultimately improving patient care and outcomes. 45-R. Early Wins: Preliminary Results of the Workforce Engagement for Compassionate Advocacy, Resilience, and Empowerment (WE CARE) intervention for Improving Nurse Well-Being Patricia A. Patrician, PhD, RN, FAAN; University of Alabama at Birmingham; Birmingham, Alabama 10/29/2023, 11:10am - 12:00pm, Breakout: 10 Nurse burnout, distress, and departure from organizations and from the field altogether remains a major concern for the field, and for individual health systems. However, organizations are still in need of evidence-based strategies to alleviate distress and foster well-being for nursing. The purpose of this study is to summarize the early results from an evidence-based wellness program, Workforce Engagement for Compassionate Advocacy, Resilience, and Empowerment (WE CARE), for nurse leaders to reduce burnout, promote resilience, and improve the work environment. Our overall design is program evaluation using multiple methods, including interviews, and repeated measures over time using surveys. A baseline survey included the Well-Being Index (WBI-9), Connor Davidson-Resilience Scale (CD-RISC-2), Mini Z (burnout), and single item measures for moral distress, work control, job satisfaction, trust in senior leadership, trust in supervisor, and intent to leave the job. The intervention includes creating a nursing-specific “Wellness Team” of six Masters-prepared RNs who engaged in unit-based rounding, and delivery of Community Resilience Model (CRM) ™ and Psychological First Aid (PFA) trainings. At baseline, nurse leaders showed the highest levels of distress, so they were targeted for the initial phase of the intervention in July 2022. A subsequent survey was administered 6-months after baseline, closing end of January 2023. The population is 3,600 RN staff and leaders who make up the inpatient nursing workforce of a large (1,200+ bed) academic health science center located in the southeastern US. This study reports on a specific intervention targeted toward nurse leaders. Here we report the preliminary results from the first 6-months of the intervention (July 2022 to January 2023) which included efforts targeted towards nursing leaders, including nursing directors, managers and assistant managers. Included in the analyses were 155 nurse leaders. From baseline, nurse leaders had a 9% improvement in overall well-being (WBI) (p=.053), a 10% reduction in symptoms of PTSD (p=.022), 12-19% a reduction of compassion fatigue symptoms (p<.001), and a 16% reduction in burnout (Mini-Z) (p=.02). Statistically significant improvements were also noted in role conflict, recognition, and culture (p<.05). Changes in resilience failed to reach statistical significance. Over 73% of the nurse leaders were aware of the existence of the WE CARE program, and 24% (n=38) of the nurse leader survey respondents indicated participating in at least one of the CRM™ trainings. Of the 38 nurse leaders that participated, over 55% indicated having used the techniques after the training. Qualitative comments indicated that in addition to practicing the techniques personally, nurse leaders were sharing techniques with their teams and implementing team-based changes based on the course. Our preliminary results indicate positive trends in the first 6 months of implementation, including high awareness of the program and benefits to participants as well as improvement in key metrics of interest. Iterative Plan-Do-Study-Act (PDSA) cycles continue to provide additional areas for improvement. The initial findings show promise for the effectiveness of nurse-led teams implementing efforts to improve well-being among nurse leaders organization-wide. Patricia A. Patrician, PhD, RN, FAAN; University of Alabama at Birmingham; Birmingham, Alabama 10/29/2023, 12:00pm - 1:50pm, Poster Session Distress among nurses has been well-documented prior to and during the pandemic, with pandemic-related trauma likely to endure for some time. To ensure a sustainable and thriving workforce, organizations must provide nursing-specific support to nurses and nurse leaders. The purpose of this project is to develop, deliver, spread, and sustain an evidence-based wellness program, Workforce Engagement for Compassionate Advocacy, Resilience, and Empowerment (WE CARE), for nurse leaders and staff registered nurses (RNs) to ameliorate or prevent burnout, promote resilience, and improve the work environment. Our overall design is program evaluation using multiple methods, including repeated measures. A baseline survey included the Well-Being Index (WBI-9), Connor Davidson-Resilience Scale (CD-RISC-2), Mini Z (burnout), Practice Environment Scale of the Nursing Work Index (PES-NWI-22), and single item measures for moral distress, work control, job satisfaction, and intent to leave the job. First, a “Wellness Team” of Masters-prepared RNs was created: 5 wellness trainers and 1 manager/coordinator. The Wellness Team received certifications in Community Resilience Model (CRM) ™ and Psychological First Aid (PFA) and are tasked with providing this training to all nursing personnel, beginning with leaders. The training was tailored to fit leaders’ schedules; stress management techniques were practiced during recurring weekly meetings with the Associate Vice President for Nursing (AVPN). The Wellness Team and AVPN developed additional interventions to influence the culture of wellness throughout the organization, e.g., Quiet Rooms were created or refreshed with new equipment. To facilitate relationship-building and spread training to nursing staff, Wellness Team members were each assigned a nursing division. The population is 3,600 RN staff and leaders who make up the inpatient nursing workforce of a large (1,207 bed) academic health science center in the southeastern US. Here we report baseline findings from the summer of 2022. Included in this analyses were 1,260 responses (66% staff nurses, 14% leaders, 20% other nurses). The majority were 25-44 years old (47.5%), female (79%), White (68%), and married (60%). Most (n=665; 62%) were in the WBI distressed category. Nearly 30% experienced moral distress at work. The average resilience score was 6.66, lower than the US adult population (M=6.91). Over 54% reported having >1 symptoms of burnout. Approximately 24% disagreed that they had control over their work. The lowest PES-NWI subscale score was Staffing and Resource Adequacy (M=2.16) and the highest score was Collegial Nurse-Nurse Relations (M=3.37). Fifty-one percent reported job satisfaction, while 40% planned to leave their job. These findings provided opportunity to implement several interventions thus far. Iterative PDSAs will provide additional areas for improvement. Because the first interventions focused on nurse leaders, we expect to see improvements in the leaders’ WBI, CD-RISC-2, and moral distress scores. As the interventions extend to staff, we will expect subsequent surveys to show further improvements. The mental health and work environment issues among nurses are so complex that no one-size-fits-all intervention can resolve. A combination of data-driven decision-making and evidence-based training and other interventions is advantageous to address organizational barriers to well-being and resilience, thereby improving the mental health of the workforce. 48-EBP. Enhancing Nursing Global Health Competencies of Undergraduate Nursing Students through A Study Abroad Experience "Down Under" Suja Davis, PhD, RN; University of North Carolina at Chapell Hill; Chapel Hill, North Carolina 10/28/2023, 2:10pm - 3:00pm, Breakout: 1 Problem, Background/Significance, Rationale: Global learning experiences provide undergraduate nursing students with opportunities to step outside of their comfort zones, adapt to new environments, and better understand global health. Further, these opportunities help students broaden their worldview and develop cross-cultural communication and critical thinking skills. Most of these experiences, however, lack theoretical underpinnings, making the design, implementation, and evaluation of theoretically grounded, evidence-based global learning experiences for undergraduate nursing students challenging. Project Goals: We aimed to provide an immersive global health experience within the Australian Health Care system for undergraduate nursing students from a large public university in the United States and analyze how student learning of specific global competencies was guided and impacted by the Nursing Global Health Competencies Framework (NGHCF) (Torres-Alzate, 2019). Methods, Implementation, and Evaluation:Torres-Alzate (2019) developed the NGHCF to guide education and research in global health nursing. Core values and principles of nursing are central to the framework, which focuses on social justice and equity, holistic care, advocacy, health as human right, sustainability, and collaboration. IRB clearance was granted for this project. After attending an information session about this international experience, interested students completed an application outlining their rationale for wishing to participate. A separate faculty committee conducted purposive sampling to ensure student diversity. The Australian host university arranged classroom, simulation lab, and clinical experiences at public and private hospitals, while the US nursing faculty accompanied students to learning activities, conducted on-site post conference discussions, and facilitated virtual reflections via Padlet©. After the experience, faculty collected and analyzed retrospective pre/post data through an anonymous, optional, online survey. Students self-reported their experience and confidence with global nursing competencies and meaningful lessons learned from studying abroad. Adapting to significantly different time zones with little turnaround time and having limited university resources to defray student costs posed barriers. Previous collaborations between the two partnering universities and exposure to an international nursing curriculum addressing social justice, equity, and Indigenous people's health facilitated the experience. Outcomes & Implications: The experience was highly impactful in promoting student competencies within the NGHSF. Student appreciation for health equity, health promotion, and healthcare systems in both countries was obvious. They learned about social justice in Australia and health outcomes while working with diverse faculty, staff, students, patients, and families. Students especially valued how simulation lab experiences promoted critical thinking and holistic nursing care, how classroom discussions addressed Indigenous health and health disparities, and how clinical experiences uncovered similarities and differences in the role of the nurse. Inter-professional collaborations were prominent throughout the experience. Nurse leaders should ensure that undergraduate nursing students have global learning opportunities to help them gain skills necessary to provide culturally responsive care as future nurses. Additionally, nurse faculty should consider planning, executing, and evaluating global learning experiences that are theoretically grounded. Our two international partnering universities will sustain the practice through the careful planning and execution of bilateral yearly immersive global experiences for undergraduate nursing students within the context of NGHSF. 49-EBP. A Nurse Leader Guide to Building an Equitable and Inclusive Nursing System Float Team: Increasing Self-Reliance and Financial Sustainability Adam Fronczek, DNP, MBA, RN, NEA-BC, ANP-BC; UCLA Health; Los Angeles, California 10/29/2023, 10:10am - 11:00am, Breakout: 8 The NSFT design is to meet operational demands and strategically expand its facilities into a centralized functional organizational structure. This allows for systematic processes and enables expansion into other areas with appropriate managerial oversight. This project’s purpose is to guide external organizations to collaborate in developing a systematic approach for redeveloping staffing models. As nurse staffing in acute care hospitals continues to evolve to meet rapid changes in healthcare, health organizations across the country have revised their operational models. Contract labor has become a principal component in staffing models, which has financially impacted organizations. As of December 2021, contract labor nurses in the United States earned as much as $8000 weekly, equating to a health system paying $24000 per month to the traveler agency. In addition, some health systems have developed an in-house float team to combat staffing problems related to future emergencies or public health threats. The NSFT strategically decided to increase in size to support adequate nursing staffing across the health system. The NSFT developed in phases, initially addressing immediate staffing needs. As the plan evolved, the team grew and expanded into different areas, which placed the organization in a position of self-reliance. The NSFT recruited highly trained RNs from other tertiary and quaternary facilities to join as per diem staff. To support the recruitment phase of the strategic plan and ensure sustainability, the per diem staff received multiple benefits, including flexible scheduling, competitive pay, equitable growth opportunities, resources, and maintaining California-mandated staffing ratios. The fiscal outlook was beneficial in many ways, including decreased costs associated with benefits, onboarding new staff, and reduced use of contract labor. The NSFT is organized into specialty divisions to allocate staff based on their experience and competency. Management coordination establishes oversight for specialty divisions to support a centralized structure and the team’s development. The assistant director for each specialty division independently provides oversight of day-to-day operations, ensuring adequate nurse staffing. The functional organizational structure ensured the NSFT workforce could grow annually, with the total team size being 907 staff as of FY23Q3, which is a growth of 33% since the merger. In addition, the design of the NSFT provides for expansion into other areas and recruits staff with the capability to deploy rapidly. The standardized model decreased costs because of increased efficiency in support structures. The NSFT reduced nursing department contract hours from 0.95% to 0.52% from 2020 to 2021. During the same period, the median contract hours for the Vizient comprehensive academic medical center compare group increased from 0.87% to 1.53%, and the 75% percentile for that compared group increased from 2.52% to 4.28%. Additionally, The NSFT’s reduction in contract labor expense contributed to an overall improvement of 6% in the nursing services department wage index adjusted per equivalent patient day. 50-R. Critical Factors for Success in Advising Doctor of Nursing Practice Students: Creating Curious, Inclusive Nursing Leaders of the Future- It’s Not Just About the Project Jeannie Corey, DNP,RN,NEA-BC; James Madison University; Harrisonburg, Virginia 10/29/2023, 3:00pm - 3:50pm, Breakout: 16 The evolution of DNP programs continues to be transformative as does faculty advisement on DNP projects. Mentoring students through project planning and execution requires keen attention to leadership competency and skill development of DNP students. Emotional and cultural intelligence, curiosity, and collaboration are essential to becoming an inclusive leader. Effective faculty advisors and evidence-based mentoring and coaching practices are fundamental to advancing DNP graduates as effective inclusive nurse leaders. Understanding faculty advisors’ lived experience of engaging DNP students in leadership practices can provide value-added strategies, tools, and actions important to successful health care systems’ outcomes. The purpose of this project is to identify critical elements of DNP faculty advising practices that support the development of leadership capabilities that are sustained beyond the DNP project. Faculty advising on DNP projects can prepare nurse leaders as they work intimately with the student in project development. While evidence exist that various models of advising have been employed, there is little on the topic of guiding students in developing nurse leader competencies during the advisement process. Nurse leader competencies can provide an overarching framework for the advising faculty to inform and support the coaching of the DNP in project and leadership abilities. A mixed methods sequential explanatory design will be used to conduct this study. Qualitative and quantitative data will be collected in two consecutive phases with results integrated to contextualize findings and results to create guidelines to implementing value-added strategies, tools, and actions for effective faculty advisement. Quantitative data will be collected through an electronic survey and will inform the qualitative component of the study which will include collecting data through taped interviews with DNP faculty advisers. Data will be analyzed to identify advising factors that lead to successful coaching and mentoring of DNP leaders. The study will identify critical elements of DNP faculty advising that supports the development of leadership acumen that goes beyond the completion of the scholarly project. Study outcomes will provide insight into successful advising strategies that may inform the development of useful tools to guide evidence -based faculty advisement for developing DNP nurse leaders. This study will integrate implementation science methods to define and operationalize advisement strategies that can be tested and applied to inclusive leadership development. 51-R. The Role of Cultural Self-Efficacy with Nurse Leaders in Promoting an Inclusive Classroom Environment Denise Morris, PhD, RN; University of West Georgia; Carrollton, Georgia 10/29/2023, 3:00pm - 3:50pm, Breakout: 17 Integration of an inclusive educational environment requires nursing faculty to embrace a transformational change in academics. The cultural interactions of an educator teaching in an urban district may differ from the relations experienced by a rural nurse educator. The purpose of this quantitative study, guided by Bandura’s Social Cognitive Theory, was to determine whether there is a difference between the cultural self-efficacy scores of nurse faculty teaching in a rural location compared to those in an urban location as well as whether the demographics of age, ethnic background, and years in the nursing profession predict cultural self-efficacy scores. Nursing faculty in seven southeastern states were asked to complete the Culturally Responsive Teaching Self-Efficacy Scales, which were distributed through social media; 68 participants responded. Independent t-test results showed no statistically significant difference between the cultural self-efficacy scores of nurse faculty teaching in a rural location compared to an urban location. Evaluation of the second research question, multiple regression results showed denoted ethnic background as the only one of three variables that significantly predicted the cultural self-efficacy scores. Further research is needed to expand the scope and composition of the participants and to enhance professional development for nursing faculty, regardless of location. Positive social change can occur in the health care system through the training of nursing students caring for diverse patient populations. 52-R. Emotional Exhaustion of nursing professionals coping with the Covid-19 pandemic: What has leadership learned? DANIELLE SARAIVA TUMA DOS REIS, Profa da Universidade Federal do Pará; Universidade Federal do Pará; Belém, Brazil 10/29/2023, 12:00pm - 1:50pm, Poster Session Introduction: The Covid-19 pandemic caused a negative impact on the nursing workforce, taking a toll on the worker's psychological health and well-being, representing a wake-up call for leadership. Objective: To identify the challenges faced by nursing leadership in the Covid-19 pandemic regarding emotional exhaustion of nursing technicians according to the dimensions of the Burnout Syndrome (BS); to highlight which work environments (wards, intensive care unit and emergency room) influenced the psychological health of these technicians and correlate working conditions with the dimensions of BS. Methods: Unpublished study carried out in the North Region of Brazil, part of a national multicenter study, with data from the pandemic period, cross-sectional, exploratory, quantitative, developed in a public hospital, with professionals more prone to infection, nursing technicians. Applied instruments tested in the five regions of Brazil, addressing socio-demographic data, work and the Burnout Syndrome. Data were analyzed by descriptive and inferential statistics performed using SPSS v.25 software. Results: Participated 152 nursing technicians, with a prevalence of female gender, brown race, mean age of 44.5 years, 16 years of professional experience, three years of work at the institution, with a weekly workload of 36 hours. The challenges faced by leadership represented a prevalence of Burnout Syndrome (BS) of 47.4% with high emotional exhaustion in nursing technicians, 42.1% with a high level of professional depersonalization and 69.1% with a low level of professional achievement without interference in the work environment. The type of employment contract and the number of professionals providing care had a direct correlation with emotional exhaustion (p=0.024; p= 0.021), while the length of experience and the number of employment contracts had a direct correlation with the Decreased Professional Achievement domain (p =0.029; p= 0.014), however it did not influence the Depersonalization domain. Conclusion: The pandemic scenario favored the signs of BS in nursing professionals, intensified by the lack of work infrastructure, equipment and professional recognition, despite this, the technicians were satisfied with the work and with the relationship established with the patients. Going forward, it is necessary to know this employee's work environment, emphasize providing support and reflection time for leaders at all levels to develop resilience, i.e., to be able to bounce back in the face of adversity, personally, organizationally and systemically. As well as respecting the humanity of the workforce, including the borders and limits that each one imposes on their role and their health, in the search for a psychologically healthy environment. 53-QI. Virtual Nurses::Investing Intellectual Human Capital Julia Aucoin, DNS, RN, NPD-BC; UNC Health Rex; Raleigh, North Carolina 10/28/2023, 2:10pm - 3:00pm, Breakout: 3 Virtual nursing comes is described in a variety of modalities. Yet examples of direct patient care are limited in the literature or in presentations. This novel model of care applied Virtual Nursing to the role of admission and discharge nurse to supplement nursing care on inpatient units. Increasingly complex admissions take longer and require focus. The virtual nurse provides an uninterrupted opportunity to learn about the patient to support completion of medication history, SDOH, and plan for discharge from admission. Patient express satisfaction with the attention provided to their needs and the thoroughness of the assessment. Patients also appreciate the details of discharge teaching and demonstrations provided by the virtual nurses. This model of care has expanded across two campuses and is being adopted across the entire system. Colleagues express they don't know how we'd make it without this team. 54-R. Quality Matters: Nurse Staffing and Clinical Outcomes Shea Polancich; Birmingham, Alabama 10/29/2023, 12:00pm - 1:50pm, Poster Session Evidence suggests better staffing positively impacts patient outcomes. During the pandemic, nurse staffing varied considerably in our academic medical center prompting our nursing leaders to question the impact of nurse staffing on patient outcomes. This descriptive study examined nurse staffing and the relationships between staffing and the quality of nursing care. On average per month, there were 6 CAUTIs, 9 CLABSIs, 68 falls, and 54 HAPIs. LOS per month ranged from 6.4 to 7.46, averaging 7 days. We observed common cause variation in CAUTIs and CLABSIs, with HAPIs and falls showing special cause variation via statistical process control. Despite the challenging factors associated with the lack of available nurse staffing that effective leadership and adherence to evidence-based quality improvement promotes and sustains positive clinical outcomes. 55-ASP. A Strong Nurse Academic Service Partnership Advances Professional Nursing and Creates Positive Outcomes Shea Polancich; Birmingham, Alabama 10/29/2023, 2:00pm - 2:50pm, Breakout: 13 The success of professional nursing is dependent on academic and service. Our academic service partnership was designed using a systematic approach organized around a strategic plan and evaluated by a formal measurement blueprint. Our nurse leaders create visionary academic programs and improve service with a strong focus on developing a nursing workforce that consistently produces quality outcomes and health system impact locally and globally. Using a structured evaluation model, we programmatically evaluate our outcomes annually. we have achieved 5 Magnet designation and our academic programs are consistently ranked in the top 20. For our 2022 reporting year, 47-65% of our pre-licensure graduates were employed within our hospital within 90 days of graduation; we had a 73.8% retention rate of RNs; 102 staff with joint academic appointments (over 1 million dollars in reimbursement); 25 reimbursed faculty practices totaling over $625,000; over $7,000,000 in partnership grant funding; 42 disseminated publications; 9 ranked programs; 6th ranked in NIH funding; a greater than 80% reduction in hospital acquired pressure injury from 2018 baseline to current 3 month average; 54 health system focused Doctor of Nursing Practice Projects; and had a greater than $7,000,000 in cost avoidance with our nurse led clinics. 56-R. Nurses’ fatigue and sleep quality and perception of the night shift work environment Susan Weaver, PhD, RN, CRNI, NEA-BC; Hackensack Meridian Health; Neptune, New Jersey 10/29/2023, 10:10am - 11:00am, Breakout: 7 Nurses in acute care settings work around the clock to ensure the continuity of patient care. Increasing evidence indicates that working day, evening, and night shifts adversely affects nurses’ physical and mental well-being and safety. Recent systematic reviews identify that shift work disrupts the sleep patterns of nurses, especially those working night shift, leading to sleep deprivation. This fatigue and reduced alertness negatively impact nurses' job performance but also significantly compromises their physical and mental health, safety, and well-being. Furthermore, it dramatically increases the risk to patient safety. As the world recovers from the COVID-19 pandemic, it is critical to promote and prioritize the health and well-being of nurses. Although studies have been conducted describing fatigue and sleep quality of nurses, there is limited research on fatigue countermeasures and the experiences of nurses working the night shift. The purpose of this study is to investigate the difference in fatigue and sleep quality between day and night shift clinical nurses, examine strategies to mitigate fatigue, and explore the night shift nurses’ perception of their experience working night shift. This mixed method study was implemented in two phases. During Phase One, nurses at a 12-hospital health care system were invited to complete a survey about their 1) quality and patterns of sleep, 2) perceptions of the severity and effects of fatigue, 3) work related fatigue, and 4) experience working night shift, for night shift nurses. In Phase Two, education sessions were held for nurses on how to manage fatigue and listening sessions with night shift clinical nurses discussing fatigue countermeasure initiatives. Responses were received from 1879 clinical nurses working at 12 hospitals in one state in the Northeast region of the U.S. On average, the clinical nurses were 38 years of age and had 12 years of nursing experience. The majority of clinical nurses held a BSN degree and worked full-time, and 50% of the clinical nurses worked during the night shift. There was a statistically significant difference between clinical nurses working day and night shift for the total score of the PSQI as well as all of its subscales, and all three subscales of the OFER Scale. This indicates that nurses on the night shift experience more acute and chronic fatigue than nurses working day shift, while nurses on the day shift have higher scores in intershift recovery, meaning they are better able to recover from work-related fatigue by the next work shift. The BFI also showed a significant difference between the two groups in all three subscales, with night nurses experience greater fatigue and interference than nurses working day shift. In the survey of nurses working night shift, more night shift nurses recalled a fatigue-related error, falling asleep at a red light, missing their exit, and having a car accident or near miss when driving home compared to day shift nurses. Therefore, there was a Call to Action for nurses and nurse leaders and initiatives will be shared on how to decrease fatigue, and improve the night shift work environment. 57-QI. Learning Health Center Leadership Makes the Case for Quality in Reducing Hospital Acquired Pressure Injury Shea Polancich; Birmingham, Alabama 10/29/2023, 12:00pm - 1:50pm, Poster Session The Learning Health System (LHS) integrates internal and external data and evidence to change processes and practices, leading to higher quality, and safer patient care. In our quality improvement study we posed the following question: Does the LHS approach create a strong case for the value of quality and safety in a health care organization? Using a descriptive observational design, we retrospectively examined longitudinal data from October 1, 2019 to March 31, 2022 using the variables of total number of all-stage HAPI counts and average length of stay (ALOS). From October 1, 2019 to March 31, 2022, the ALOS ranged from 6.40 to 7.46, an overall average of 6.97 for the time period. HAPI counts ranged from 17-107, overall average of 53.6 for the same time period. HAPI per 1000 patient days for FY 20 (October-September) and FY 21 decreased from 2.30 to 1.30. A statistically significant, strong negative correlation, r = .524, P = .003, was found using correlation analysis. The LHC efforts directed toward HAPI reduction have led to sustained improvements spanning multiple years despite the decline in quality outcomes nationally. 58-R. The Impact of Span of Control on Nurse Managers and Hospital Outcomes Asiah Ruffin, BSN, RN; University of Alabama at Birmingham; Birmingham, Alabama 10/29/2023, 12:00pm - 1:50pm, Poster Session Span of control is a concept that must be better understood in healthcare and nursing contexts. Nurse managers with excessive spans of control are at an increased risk for poorer outcomes and unit performance. Heavy workloads and job pressures have become normal since the coronavirus pandemic. The current span of control practices limits the effectiveness of nurse managers and hinders quality outcomes. Poor work environments diminish nurse managers' ability to build relationships and maintain communication, widening the gap between management and staff. Today’s nursing workforce requires strong and adaptable leaders. However, nurse manager leadership effectiveness is restricted as they supervise many direct reports and balance a range of varying tasks. This concept analysis aimed to determine factors associated with nurse manager span of control and to provide a comprehensive definition outlining the depth of this concept. This concept analysis aimed to examine factors associated with nurse manager span of control and introduce a comprehensive definition of this concept. An adapted Rodger’s evolutionary approach guided this concept analysis. Proquest, PubMed, and Scopus databases were searched for peer-reviewed literature addressing span of control in acute care nurse management. Data from 22 articles were included in this concept analysis. This concept analysis includes antecedents, attributes, and consequences of excessive nurse manager spans of control. Work-related factors, including staff and manager experience levels, work complexity, and patient acuity, are attributes of a nurse manager's span of control. Findings from this concept analysis suggest that excessive spans of control can contribute to role overload and burnout among nurse managers, poor satisfaction among staff and patients, and increased costs for healthcare organizations. The attributes presented in this concept analysis shed light on the complexity of acute care nurse manager roles and responsibilities. Defining the span of control for acute care nurse managers position future researchers to measure various aspects of a nurse manager’s role, thereby laying the foundation to create practical solutions to optimize the span of control practices in acute care facilities. An inclusive assessment of a nurse manager’s workload will assist hospital administrators in making informed, evidence-based decisions, increasing the odds of better patient and organizational outcomes. 60-R. Factors Influencing Direct Care Nurses Intent to Leave and Implications for Retention Melissa Miller, PhD, RN, CNOR; Womack Army Medical Center; Fort Bragg, North Carolina 10/28/2023, 2:10pm - 3:00pm, Breakout: 3 Factors influencing direct care nurses' intent to leave, and retention-related perceptions were exacerbated by the global pandemic and the on-going nursing shortage. Addressing these factors necessitates a systemic response. This response requires healthcare organizations to garner a comprehensive understanding of these factors. A team of researchers representing a federal, clinical-academic partnership, explored direct care nurses’ perceptions within the Military Health System to better understand nurses’ perceptions of the factors influencing their intentions. This presentation details the findings from a content analysis exploring 1, 483 free-text comments to a broad prompt at the conclusion of the Military Nursing Practice Environment Surveys conducted in 2016 and 2018. Findings suggest leadership and management relations, career and professional development opportunities, staffing, communication, and work environment are likely to influence direct care nurses’ retention-related perceptions and intent to leave. Several known reasons for potentially preventable loss may be amended to address nuances and additional reasons may be included for future evaluations. The continued evaluation of potentially preventable loss through quantitative and qualitative methodologies was supported. New knowledge regarding nurses’ retention-related perceptions may inform the development of evidence-based strategies to influence nursing retention across the Military Health System. The success of this study supports leveraging similar academic-clinical partnerships amongst military treatment facilities (e.g., hospitals, clinics, etc.) and academic institutions for the continued evaluation and performance improvement of the Military Health System. 61-R. Burnout Syndrome in Nursing Technicians in Intensive Care: the impact of the Covid-19 Pandemic Liana Amorim Correa Trotte, Assistant Professor; Universidade Federal do Rio de Janeiro City: Rio de Janeiro; Rio de Janeiro, Brazil 10/29/2023, 2:00pm - 2:50pm, Breakout: 14 Problem: Burnout Syndrome is classified as a psychosocial occupational disease characterized by high-stress levels. During the Covid-19 pandemic, nursing workers experienced a state of calamity in the country, with a lack of structure in the public health network, financial insecurity, high patient mortality, risk of acquiring the disease, and work overload. Therefore, the importance of highlighting the subject is evident, stimulating a more humanized view of these professionals. They are also people with insecurities, fears, and limitations that they adopt physically and mentally, especially in a pandemic context. Objective: To evaluate the burnout syndrome in an intensive care unit nursing technicians to care for patients with covid-19. Methods: This study uses a mixed methodological approach guided by the Mixed Methods Appraisal Tool instrument. The study setting was the intensive care unit of a public university hospital in Rio de Janeiro - Brazil. The sample consisted of nursing technicians who observed direct care for patients with Covid-19 between April and June 2021. The Maslach Burnout Inventory (MBI) and a semi-structured interview were used to learn about facilitating and protective factors related to Burnout. Quantitative data were analyzed using SPSS software version 25.0. The qualitative data were submitted for content analysis using the Interface de R pour Analysis Multidimensionnelles de Textes et de Questionnaires (IRaMuTeQ) software. Results: The sample consisted of 51 nursing technicians, 74.5% women, 63.2% black, and 68.6% worked during the day and had more than one job, with a mean age of 39.9. The results indicate that 11.8% of the participants have high levels of Emotional Exhaustion, 21.6% increased levels of Depersonalization, and 19.6% low levels of Professional Achievement. Qualitative data showed factors that contribute to these percentages, such as the clinical condition of the patients, emergencies and deaths in total numbers, and complex work dynamics. On the other hand, the protective factors highlighted were gratitude regarding the working conditions, a good relationship between the team, and recognition of their work considering the clinical aspects and their bio-psycho-spiritual needs. Relevance to the topic: The prevention and treatment of burnout syndrome go beyond the individual benefits of professionals, reflecting on the work environment and better performance of organizations. The results can influence organizational management and support better leadership practices. Learning objectives: To evaluate the occurrence of burnout syndrome to improve organizational management in adverse situations and; To evaluate the professional practice environment for the health and well-being of the nursing workers. 62-ASP. Sustaining Patient Experience Care Transition Metrics: Leveraging Academic Practice Partnerships Shannon Layton, DNP, RN, LICSW, NEA-BC, CNL, CNE,; University of Alabama at Birmingham School of Nursing; Birmingham, Alabama 10/29/2023, 12:00pm - 1:50pm, Poster Session Abstract Background and Purpose: The Birmingham VA Health Care System care transition performance metrics performed poorly when benchmarked against other regional and national facilities. An inclusive and diverse interprofessional team led by a VA Quality Scholar (VAQS) identified several opportunities for improvement including increasing Veteran engagement and knowledge retention with the discharge process. The primary aim of this project was increasing Veteran care transition experience scores from the lowest quintile to the fourth quintile nationally over one year. A secondary aim was creating a mechanism to sustain improvement that included leadership opportunities. Abstract Methods: The Model for Improvement was selected as the framework for implementation of the four-phase project. Phases 1-3 consisted of establishing an interprofessional workgroup to conduct rapid cycle quality improvement (RCQI) to develop and streamline an evidence-based Veteran and caregiver discharge bundle. This included a discharge journey board and companion website created to enhance knowledge retention. An additional diverse and inclusive Veteran committee was formed to provide stakeholder feedback. These actions improved Veterans’ experience with discharge planning; however, initial use of a third-party vendor was not sustainable to support the discharge journey board and website. We sought additional sustainment opportunities, creating a phase 4 partnership between the VAQS fellowship program, the VA Post Baccalaureate Registered Nurse Residency program (PB-RNR), and facility nurse leaders. Key stakeholders from each group were identified to continue this work. The PB-RNR Residents completed nine literature reviews and designed nine webpages to support the discharge journey board website. Abstract Evaluation/Results: Quarter 4 FY2021 care transition scores improved nationally, increasing from the 5th (48) to 3rd quintile (79). Qualitative data from leadership rounds affirmed positive Veteran engagement with the DJB and website. Veterans reported satisfaction with DJB delivery and content. PB-RNR Residents found opportunities to participate in project sustainment meaningful and engaging. Residents participated in RCQI completing 9 EBP practice projects. A diverse and inclusive interprofessional care transition improvement team continues RCQI and bundle implementation across the facility. Abstract Implications: Veteran experience score improvements can be monitored and sustained through an academic practice partnership. In addition, nurse residents completed meaningful EBP projects while leading and engaging in work that supports organizational and Veteran needs. 63-ASP. Innovation Ignite! Preparing Nurse Leaders for engagement in Health Services Innovation Roberta Pawlak, PhD, RN, NEA-BC; University of Wisconsin - Madison; Madison, Wisconsin 10/29/2023, 12:00pm - 1:50pm, Poster Session Innovation in health services can take many forms. Rapidly changing environments require nimble nurse leaders that understand the need for efficient operations, as well as acknowledgment of influences on the health care market that control access to care and payment for services. This regulatory and market environment incentivizes leadership to prioritize areas of focus in quality, efficiency and evidence-informed practice. Many of these influences require an understanding of the spectrum of innovation in health services. Often nurse leaders are not formally prepared with the tools and processes of innovation, and therefore may not engage actively in igniting the innovation spark in the systems they lead. This presentation will introduce a partnership with innovation resources at the University of Wisconsin-Madison, and detail how the Doctor of Nursing Practice (DNP) program in Systems Leadership & Innovation works collaboratively with university and industry connections in preparing future nurse leaders. Shared examples of student outcomes and lessons learned in continuous improvement demonstrate the importance of identifying resources for innovation skill growth in nursing leaders. 64-EBP. Leading Change: Moving from Quality Improvement to Research to ensure Scale-up and Spread of Evidence-based Practice Mary Dolansky, PhD, RN; Case Western Reserve University; cleveland, Ohio 10/29/2023, 12:00pm - 1:50pm, Poster Session Age-Friendly Health Systems (AFHS) (Institute for Healthcare Improvement (IHI)) is defined using an evidence-based framework, the “4Ms” – What Matters, Medication, Mentation, and Mobility. The objective of the presentation is to describe the use of quality improvement and research to reliably deliver of the Age-Friendly Health System (AFHS) 4Ms Framework in the over 1,200 MinuteClinics across the country. The Model for Improvement, Consolidated Framework for Implementation Science (CFIR), and the RE-AIM implementation frameworks were used during the pre-implementation phase, quality improvement methods were used to guide the integration of implementation strategies during the two year implementation phase and research methods were used to scale up and spread in year 3. The MinuteClinic in year one achieved Committed to Care Excellence for all regions and in year 2 achieved 21% uptake of all 4Ms including 700 of the 1100 clinics demonstrating preliminary uptake of the evidence-based practice 4Ms into care delivery. Significant improvements were noted for all 4Ms (What Matters, Medications, Mentation, and Mobility, p<0.05 when comparing the intervention to baseline time periods. In year 3, the Virtual Clinic pilot research study found an increase in confidence in completing assessments and act-ons and a significant difference in delivering the 4Ms after playing the game compared with those who did not play. The Reflection and Action demonstrated significant changes indicating preliminary evidence to test the interventions on a larger scale. The results of the larger-scale research studies will be reported in the fall. 65-QI. Introduction of an Innovative Care-Based Delivery Model Tracey K. Dick, PhD, RN, CNE, COI; UAB School of Nursing; Birmingham, Alabama 10/29/2023, 12:00pm - 1:50pm, Poster Session Background and Significance: Quality, safety, and cost continue to require prioritization in health care delivery. The COVID-19 pandemic challenged staffing models used in acute care. There is a pressing need to identify sustainable care models that optimize health care delivery while balancing clinical and financial outcomes. Testing of an innovative care-based delivery model aligns with current operational needs at University of Alabama at Birmingham (UAB) hospital. Project Goals: The goals of this project are to improve staff satisfaction, perceived adequacy of unit staffing, intent to leave, and satisfaction with teamwork, communication, and delegation skills by implementing an innovative care-based delivery model on one unit at UAB hospital. Methods: A PDSA Model for Improvement methodology is being used to implement and evaluate a care-delivery model focused on differentiated practice that employs PCTs, LPNs, and RNs working together collaboratively, and communicating openly to deliver care to the patients. This model will extend the work of the RN through teamwork and delegation to the appropriate nursing personnel based on scope of practice, licensure, and level of competency. The project includes a change in staff skill mix, evidence-based training using the Agency for Healthcare Research and Quality TeamSTEPPS® curriculum, and custom simulations to support this differentiated practice model. Evaluation Plan: Using Donabedian’s Structure-Process-Outcome Framework, staffing and skill mix measures will represent the structure variables; process variables will include staff participation with TeamSTEPPS® education, missed nursing care, teamwork, communication, and delegation; and outcomes will include staff satisfaction, intent to leave, cost, satisfaction with teamwork, and perceived adequacy of unit staffing. Pre-implementation data was collected using the MISSCARE (Kalisch & Williams, 2009) and Nursing Teamwork (Kalish et al., 2010) surveys. Those two surveys will be used to collect data every three months to measure missed nursing care, communication, staff satisfaction, intent to leave, satisfaction with teamwork, and perceived adequacy of unit staffing. Administrative data will be used to determine organizational cost and quality metrics. Periodic reflections with unit staff members and leadership will provide qualitative data to inform the RNs’ development of delegation skills. Unit observations will also be performed with a project-specific unit observation tool guiding evaluation of task/role delineation within the unit. Outcomes: This project is currently in progress. 66-ASP. Financial Toxicity: The Importance of Understanding the Cost of Health Care Lyn Stankiewicz Losty, PhD, MBA, RN; Walden University; Corolla, North Carolina 10/29/2023, 11:10am - 12:00pm, Breakout: 11 Research has posited that quality health care is a right for every person, yet there are different perspectives in terms of how “quality” health care is defined and delivered (Ranabhat & Jakovljevic, 2023). For example, according to the Agency for Health Care Research and Quality (AHCRQ), the basic domains of quality healthcare include effectiveness, efficiency, equity, patient-centeredness, safety, and timeliness (AHCRQ, 2023). The World Health Organization described the basic principles of health care as the right care, at the right time, responding to the service users’ needs and preferences, while minimizing harm and waste (WHO, 2023). Along with these principles, there is also considerable debate over whether quality health care comes at an additional cost. Research has demonstrated there are “substantial psychological, social, behavioral, and health-related impacts of the rising costs of health care” (Hamel et al., 2016), which has become to be known as financial toxicity. Financial toxicity is described as the cost-related hardship and associated burden of healthcare costs on patients (Politi et al, 2023), and is often associated with delaying necessary care, skipping prescribed medications, and even influencing mortality (Ramsey et al., 2016). While financial toxicity is considered an international concern, it has been identified as a major concern in the US given the lack of universal insurance coverage compounded with high out-of-pocket costs for those with insurance (Carroll, 2022). Politi et al. (2023) posited that most providers do not initiate or engage with cost discussions with their patients even though many patients feel the need to ask questions about the cost of care. One reason for this may be the lack of knowledge and awareness surrounding the actual cost of care and care delivery. Interestingly, research has demonstrated that a discussion regarding cost of care as part of the patient’s decision-making process can improve patient and organizational outcomes (Ubel et al., 2013). As a result, it is imperative that nurses and nurse leaders are not only aware of financial toxicity but are aware of strategies to ensure this important discussion takes place to ensure equitable and inclusive healthcare delivery to the patients that they serve. 67-R. A Pathway for Gender Equity in Healthcare: Solutions for Health Leaders Sonia Udod, RN,PhD; University of Manitoba; Winnipeg, Canada 10/30/2023, 10:35am - 11:30am, Breakout: 20 A commitment to gender equity in healthcare leadership begins with senior leadership. Health leaders need to be well positioned to address issues in a shifting context and chaotic workplace. The context has been exacerbated by a pandemic resulting in the strain, compassion fatigue, and burnout experienced by a dwindling, traumatized, and exhausted nursing workforce. One feature of this context is the disproportionate burden on women, who make up the majority of health leaders and nurses, while often balancing home responsibilities. Gender roles, relations, norms, and expectations shape the progression of equitable processes by health leaders at multiple levels. Increasing leadership capabilities and leadership pathways for women is an opportunity to further health system resilience and system responsiveness while building equity and justice into the employment system for women. As part of a larger study on crisis leadership and organizational resilience during COVID-19, we explored how health leaders fostered organizational resilience and how that may be shaped by attention to gender equity and gender relations, norms, and expectations to inform action. The qualitative exploratory research design consisted of criterion sampling of 14 senior health leaders and 10 frontline managers, across three health regions in Manitoba, Canada. Participants completed socio-demographic questionnaires and individual semi-structured interviews. Data were analyzed using Braun and Clarke’s six-phased approach to thematic analysis guided data analysis to explore how senior health leaders and frontline managers fostered organizational resilience and how that may be shaped by gender relations, norms, and expectation in fostering gender equity. Four main themes were identified in terms of how health leaders and frontline managers understood and took action that fostered organizational resilience and how that may be shaped by gender to inform action: (1) challenges faced (e.g., retraumatization), (2) shifting power through relationship building, (3) compounding stress at home and work; (4) shifting expectations of what resilience means. We conclude by discussing how workplaces may justify different expectations and opportunities for women that are often reinforced by family roles and cultural practices that affect gender norms and relations at the institutional level. In the context of a crisis, gendered roles, gender equity and leadership play a prominent role. Attending to gender differences is important for leaders and managers to address and aligns with creating workplace cultures that ease family demands (i.e., workplace childcare) for women that can improve organizational performance to drive quality patient outcomes. These findings have implications for those in existing positions of leadership and serve as a catalyst for organizational resilience to foster capacity in building equity and justice for women employed in the healthcare system. 68-R. Examining the role of nursing leadership in Brazilian university hospitals in the COVID-19 crisis José Luís Guedes dos Santos, PhD, RN; Universidade Federal de Santa Catarina; Florianópolis, Brazil 10/30/2023, 10:35am - 11:30am, Breakout: 19 The aim of this study was to investigate the role of nursing leadership in Brazilian university hospitals during the COVID-19 crisis. It was a cross-sectional study carried out in 10 Brazilian university hospitals during the COVID-19 pandemic. A total of 1376 participants were included. Data were collected through an online questionnaire between March and December 2021, including sociodemographic and labour information. The Leadership Indicators from the Nursing Work Index Practice Environment Scale (PES-NWI) was used to measure nursing leadership. Most participants were female with an average age of 40 and 13 years of professional experience. The workload was found to be around 34.82 hours per week, and most participants did not have another employment relationship. Despite feeling that the number of nursing professionals for care provided was inadequate, the majority of participants reported being highly satisfied with their current job. The PES Leadership was positively evaluated by all three groups. The study also found a positive correlation between the PES Leadership and work satisfaction and intention to leave the job. These findings suggest that healthcare institutions should prioritize leadership development to improve nursing professionals' job satisfaction and retention. 69-EBP. Building Nurse Entrepreneurs for an Equitable Future John FitzGerald, MA in Psychology, Organizational Behavior concentration; Case Western Reserve University; Cleveland, Ohio 10/29/2023, 3:00pm - 3:50pm, Breakout: 18 This submission aims to advance nurse entrepreneurship through an evidence-based approach. Nurses are well-positioned to start healthcare-related businesses, yet the prevalence of entrepreneurial nurses is low. The submission highlights the need for more emphasis on nurse education in entrepreneurship and the societal taboo associated with nurses charging for their services. The Marian K. Shaughnessy Nurse Leadership Academy, in partnership with the Veale Institute for Entrepreneurship at Case Western Reserve University, has established an innovative program known as Executive/Entrepreneur in Residence. The program's primary goal is to offer exceptional opportunities for students, faculty, and alumni to learn and grow from the wealth of experience and expertise of selected nurse entrepreneurs. The programming has yielded positive outcomes and feedback, and this submission presents the evaluation plan and outcomes of the pilot program with two nurse entrepreneurs in residence. Over the course of these two residencies, nearly 200 faculty, students, and alumni engaged in entrepreneurial education for nurses. 70-ASP. Who are nurse leaders? How do we know? Roberta Pawlak, PhD, RN, NEA-BC; University of Wisconsin - Madison; Madison, Wisconsin 10/29/2023, 12:00pm - 1:50pm, Poster Session Within the fast-paced demands for health services along the continuum of care, nurse leaders need to adapt rapidly to meet system needs. In this adaptation, we may lose sight of our nursing practice discipline and theoretical underpinnings. Further, as we specialize in nursing leadership, the chasm between our leadership competencies and standards (AONL, 2023; AACN, 2021) and “who we are as a nurse”, or the theoretical foundation of nursing, can become less connected. Educating future nurse leaders in a DNP Systems Leadership program and tying their future practice to both practice theory as well as professional practice standards and competencies became a challenge. One solution was to integrate a connection through study, application, and a “Letter to My Future Self.” Future leaders were asked to connect Middle-Range and Situation-specific Theories to nursing leadership standards and competencies, and ‘envision’ who they would become in future roles. The initial qualitative feedback from the students communicated a theme of appreciation and relationship with nursing theory, as it informed their past and current practice experiences, as well as value in connecting with professional competencies in leadership in current and future state. The mechanism for connection (tool) will be discussed, as well as feedback from future leaders as they envisioned themselves as a “NURSE” leader in future state. 71-ASP. Challenging assumptions in the quest for equitable maternal child health Candace Knight, PhD, RN, FAAN; University of Alabama at Birmingham School of Nursing; Birmingham, Alabama 10/29/2023, 12:00pm - 1:50pm, Poster Session This academic nursing practice partnership led to improved maternal child health outcomes in the local community, policy changes and funding opportunities at the state level, clinical experiences for interprofessional students in population health, and challenged assumptions of clinicians and students alike regarding vulnerable populations. 72-QI. Oral Care to Decrease Non-Ventilator Associated Hospital-Acquired Pneumonia Susan Kill, MSN, RN, NEA-BC, CNRN; University of Alabama at Birmingham; Birmingham, Alabama 10/29/2023, 12:00pm - 1:50pm, Poster Session Hospital-acquired pneumonia (HAP) is responsible for 25% of all hospital-acquired infections. HAP increases mortality rates, length of stay, admissions to intensive care units, the use of mechanical ventilation, and costs. Ventilator-associated pneumonia, a subset of HAP, has been very well managed in the ICUs over the past two decades. However, the incidence of non-ventilator associated (the second subset of HAP) has not improved since the early 2000s. Non-ventilator associated pneumonia (NV-HAP) is now more costly, more deadly, and more prevalent than ventilator-associated pneumonia. NV-HAP is avoidable with evidence-based oral care nursing interventions. Bacteria are the main cause of HAP. Hospitalization precipitates changes in the colonization of dental plaque. The presence of bacterial biofilm on the surface of teeth and on the oral mucosa allows bacteria to colonize. Microaspiration occurs, allowing the bacteria to enter the upper airway and lower respiratory tract. Colonization of the oropharynx is affected by co-morbidities such as chronic malnutrition, alcoholism, and diabetes. Risk factors include age, chronic obstructive pulmonary disease, asthma, structural lung disease, bronchiectasis, cardiovascular disease, heart failure (HF), cardiomyopathy, acid-base imbalances, renal disease stroke, epilepsy, Parkinson’s Disease, dementia, and other neurodegenerative diseases. In 2011, an interdisciplinary team launched the Hospital-Acquired Pneumonia Prevention Initiative (HAPPI) after a thorough literature review. The team determined that the most easily modified risk factor was to decrease the bacterial pathogens in oral biofilm and implemented a universal, enhanced oral care protocol. The HAPPI project achieved a statistically significant reduction in HAP rates over four years, a cost avoidance of $4.5-6.5 million dollars (164 cases avoided), and developed an oral care protocol for acute care hospitalized adult patients that was ratified by the American Dental Association. Oral care became standard work. Other HAP reduction programs were initiated with similar results. This DNP Project will utilize the IHI Improvement Model to implement an oral care protocol in three inpatient units. Each of the three implementation units will receive education on oral care and NV-HAP, as well as training on toothbrushing techniques. The Influencer Model will be utilized to reduce the potential for “improvement evaporation” and assure the long-term sustainability of the universal practice of oral care. The measures for this quality improvement project include staff training, knowledge attained, oral care provided, oral care socialized as a valued intervention, oral care documented, the incidence of HAP, oral care as standard work, staff perception, and the financial impact of a reduction in HAP. The implementation team will collect observation and medical record data, and Qualtrics surveys will be sent to the staff to collect staff perception data. Data will be input into SPSS for descriptive analytics. This project will be deemed successful when the outcomes replicate the outcomes of the QI projects referenced within this project, there is a reduction in the incidence of HAP, and there is universal acceptance and sustainment of the oral care protocol on a routine daily basis. 73-R. Faculty Decisional Involvement Scale Development Nancy Ballard, PhD, RN, NEA-BC; Kennesaw State University; Kennesaw, Georgia 10/29/2023, 12:00pm - 1:50pm, Poster Session Shared governance in academic settings has been in place since the mid 1960’s when the role of faculty in university decision making was legitimized with a formal statement from the American Association of University Professors, American Council on Education, and the Association of Governing Boards of Universities and Colleges entitled, “Statement on Government in Colleges and Universities.” While shared governance has been embraced by universities and colleges, satisfaction with faculty involvement in areas outside of academic policy is a desired area of improvement among faculty. Formal shared governance structures at the university level vary regarding how well processes work to support collaborative decision making and may lead to slowed resolution or adversarial situations. Pearce, et al. (2018) posited a transition to a shared leadership model which uses a task force approach based on needed expertise and minimal use of councils might be a better solution than a representative council structure for all decisions. Faculty led committees in the school of nursing and other departments commonly deal with academic policies/issues, promotion and tenure, applicant review for faculty positions. Anecdotally, faculty state they would like a more active role in decision making regarding decisions in other areas. Use of shared leadership supporting collaboration at the department level in universities has had limited study. Lack of clarity regarding areas in which faculty would like more involvement supports a need for this research. The purpose of this study is to evaluate nursing faculty’s perception of actual vs. desired decision making at the department level using a Faculty Decision Involvement Scale (FDIS) modeled after a widely used staff nurse Decisional Involvement Scale (DIS) developed by Havens and Vasey (2003). The 21-item FDIS was developed using a two round-reactive Delphi Process which included review by four experienced faculty from different universities. Content Validity Index (CVI) analysis revealed a CVI of 0.75 or higher on most items. Locally, data will be used to inform plans for restructuring decision-making processes in the school of nursing. Following the pilot administration of the instrument to a department of nursing, items will be re-evaluated. Once the final tool is established, additional participants will be recruited from other departments at the university. Further expansion of the study to other universities will be explored. 74-QI. Staffing by Acuity – Myth or Reality? Program evaluation of an EHR imbedded Nursing Workload Acuity Tool using ANA’s Principles for Nurse Staffing Ida Anderson, MSN, RN, NEA-BC, ONC; UCLA Health; Los Angeles, California 10/29/2023, 3:00pm - 3:50pm, Breakout: 18 Objective nursing workload acuity information is vital to ensure equitable distribution of nursing resources. Hoogendoorn et. al. (2021) proposes that it is more important to focus on nursing workload than nurse to patient ratio. However, it is becoming clear that while objective nursing workload acuity tools can provide useful information, they often do not impact the organization’s ability to staff patient care areas with the necessary nursing resources based acuity (Bruyneel et.al., 2019). Perceived high workload is associated with nurse burnout and job dissatisfaction and if left unaddressed can significantly impact stability in nursing teams. When a mismatch exists between the objective nursing acuity tools and the available staffing resources, nursing confidence in the ability to provide safe care is negatively impacted (Eastman & Kernan, 2022). Therefore, a detailed program evaluation of UCLA Health’s existing nursing workload acuity tool will provide meaningful and important information for all nurse leaders who plan resources for their teams. 75-R. Educational Pathways of Nurse Practitioners who work in Emergency as Predictors of Competence and Capability Deborah McCrea, EdD, MSN, APRN, FNP-BC,CNS, CNE,CEN, CFRN, EMT-P; UTHealth School of Nursing at Houston; Houston, Texas 10/29/2023, 2:00pm - 2:50pm, Breakout: 14 Background: Research on educational needs of nurse practitioners (NPs) who work in emergency settings suggests that the emergency department (ED) is a very complex and unique setting. NPs who choose to work in this setting are required to have a particular education and skills to meet the demands of working in the ED. Currently, there are three major educational pathways for NPs to work in an ED: On-the-job experience, university-based postmaster’s emergency programs, and postmaster’s emergency fellowships. However, there are no national or state regulatory mandates on the educational background that is needed to function as an NP in this setting. Purpose: The following research questions guided this study: (1) Do educational pathways of family nurse practitioners who work in an emergency setting affect perceptions of competence and capability? (2) Are these perceptions of competence and capability of nurse practitioners who work in an emergency setting affected by prior professional experiences working in an emergency setting as a registered nurse (RN) and prior experience working in the NP role in any setting or specialty? (3) How do NPs in emergency settings perceive the complexity of their role during their first month and twelfth month on the job? Methods: This study recruited 215 NPs from several NP organizations, social media, and snowball sampling. Of these participants, 153 had on-the-job training, 44 had a university-based emergency program, and 18 had emergency fellowship program qualifications. An online survey with MANOVA was used to answer research questions 1 and 2, while the Wilcoxon signed-rank test was used to answer research question 3. Results: On educational pathways, MANOVA revealed there were statistically significant differences among the three educational pathways on three competence subscales: cardiovascular (p=.28), musculoskeletal (p=.24), and nervous system (p=.47). However, no statistical difference was found on the combined capability subscales. On years as an RN in an ED, NPs with less than one year of experience reported lower resuscitation 76-R. PRACTICE ENVIRONMENT AND NURSING CARE DURING THE PANDEMIC IN THE AMAZON CONTEXT DANIELLE SARAIVA TUMA DOS REIS, Profa da Universidade Federal do Pará; Universidade Federal do Pará; Belém, Brazil 10/29/2023, 12:00pm - 1:50pm, Poster Session Introduction: The work context in the midst of the pandemic brought as a challenge the nursing care in a fragile hospital practice environment in the Brazilian Amazon. The assessment of care is an indicator to support the nurses´ work, who, as team leaders, need to ensure the quality of the care provided. Objectives: To measure the professional nursing practice environment through the Practice Environment Scale – PES instrument, and the care product through the APROCENF instrument in hospitals in the Brazilian Amazon. To correlate the two instruments PES and APROCENF in the pandemic scenario. Methods: Quantitative, cross-sectional, descriptive study, part of a multicenter project developed in three federal public hospitals in the Brazilian Amazon in the states of Pará, Mato Grosso and Amazonas, which serve medium and high complexity by the Unified Health System. Nurses from hospitals who provided care for at least 3 months to patients diagnosed with Covid-19 participated. Applied the Practice Environment Scale - PES and APROCENF instruments and performed descriptive and inferential statistics in the SPSS v.25 software, using the chi-square, Mann-Whitney, Pearson correlation and Cronbach alpha tests. Results: 129 nurses participated, with a prevalence of females (78.3%), brown race (63.6%), with a mean age of 42.2 years, 15 years of professional experience, seven years of work in the institution, with a weekly workload of 36 hours. The environment of professional nursing practice was considered favorable in all hospitals (p=0.001). The product of nursing care, AM stood out with the classification GOOD (59.1%) to GREAT (27.3%), as well as the distribution of the sum of responses between environments, which was significant (p=0.022), with higher distribution of scores in AM (median=28) when compared to MT and PA (median=23.5 and 23.0 respectively). The correlation between the APROCENF scores and the PES subscales showed a Strong (0.817) reliability level for AM and Regular for MT (0.539) and PA (0.604). Conclusion: The pandemic scenario represented by high cases of Covid-19 exposed the weaknesses in public hospitals in the Amazon, while at the same time rescuing the need for quality patient care as a result of a favorable environment for nursing practice, essential factors to subsidize the knowledge and planning of leadership actions for the proper management of human resources in nursing. 77-EBP. A Program Evaluation of the Atrium Health Mentoring Program for Women on the Road to Success (MPWRS) Patricia Mook, MSN, RN, NEA-BC, CAHIMS, FAONL; Advocate Health; Charlotte, South Carolina 10/29/2023, 12:00pm - 1:50pm, Poster Session There is considerable evidence that a mentorship approach to leadership development can positively affect both individuals and organizations. Formal mentoring programs have become a popular tool among United States organizations. This program evaluation will assess the Atrium Health MPWRS Program’s outcomes. The evaluation will identify opportunities for improvements and make recommendations from evidence-based practice for future performance to determine the value of expanding the program. 78-R. Mentoring clinical nurses with new approaches Kimberly Knotts, MSN, RN, NEA-BC; Wellstar Paulding Medical Center; Hiram, Georgia 10/29/2023, 10:10am - 11:00am, Breakout: 7 Introduction: This project began with the goal of mentoring clinical nurses who had completed their initial orientation program through a focused educational intervention supported by monthly face to face meetings. The program was conducted during the pandemic which necessitated additional support to the participants. The role transition from student to new graduate registered nurse is often a difficult one. Achieving competency and proficiency as new graduate nurses can be a challenge. Clinical mentors for this study were experienced clinical nurses who served as role models for these new nurses. This research study educated mentors and mentees about nurse-to nurse mentoring, utilized the Mentoring Up Theory, and explored experiences of mentors and mentees participating in the pilot study. This program provided support through a pilot clinical nurse mentoring program through structured education, tools, and evaluation. In addition, focus group results provided additional information on the benefits of the mentoring program. Methods: The participants began the mentoring program with an educational session. Mentors and mentees completed the consent form, a demographic tool, a pulse survey at the mid-point of the program and participated in focus groups. In addition, 90 days after the study, the participants will be asked to complete a post-assessment tool. Leaders in the organization who have had a staff member participate in the program will be asked to complete an evaluation tool about the program at the end of the study. The leaders will be sent a consent form and the evaluation tool at the completion of the program. Feedback from the participants will be used to evaluate the mentoring program's effectiveness as well as contribute to future large scale mentoring programs in the health system. Results: Structured monthly communications and face to face direct support by the research team members enabled the participants to continue in the program despite pandemic surges. In addition, the mentor and mentee pairs found creative ways to communicate given their inability to meet in person during covid which was perceived as a strength. Future programs will incorporate and evaluate these principles to evaluate the effectiveness of mentoring. Even participants who were unable to fully participate in their mentor/mentee pairs felt supported through the communication and support they received. 79-R. Patient Experience during the COVID-19 Pandemic Patricia Patrician, PhD, RN, FAAN; University of Alabama at Birmingham; Birmingham, Alabama 10/29/2023, 12:00pm - 1:50pm, Poster Session Research Objective To determine patient experience subscales as predictors of overall hospital rating and likelihood to recommend the hospital among COVID-19 patients versus non-COVID-19 patients. Study Design We retrospectively evaluated cross-sectional HCAHPS patient experience data during the first wave of the COVID-19 pandemic. We coded the data using Likert scaling (1= never to 4 = always) rather than proportions of patients who responded in a certain way. We used propensity matching by demographics characteristics and ran linear regressions to predict overall hospital rating and likelihood to recommend the hospital. Population Studied The population included all 3,636 discharged patients who completed the HCAPHS survey between March and December 2020.The setting for this study was an urban academic health science center located in the southeastern United States. Principal Findings Patients with COVID-19 (n=104) differed from those without a COVID diagnosis (n=3532) on the following demographics: race, risk of mortality (ROM) and severity of illness (SOI). COVID patients were more likely to be African American and Hispanic, at higher ROM, and with increased SOI. COVID-19 patients scored lower on all subscales of HCAHPS subscales and individual items. Most were statistically significant except for doctor communication, nurse communication, discharge information, and care transitions. Following propensity matching, all subscales and single HCAHPS items were statistically significantly related to overall hospital rating; the largest estimate and t-statistic was for nurse communication (est.=1.28, SE=0.18, t=6.99, p<.001). In this model, COVID diagnosis was not associated with overall rating. The model predicted 61% of the variance in overall hospital rating. For likelihood to recommend the hospital, the results were somewhat different in that care transitions, and hospital cleanliness and quietness at night were not associated with likelihood to recommend. Again, nurse communication had the highest t-statistic (t=5.76, p<.001). COVID-19 diagnosis was however, associated with a lower likelihood to recommend (t=-2.12, p<.03). The adjusted R-square in this model was .44. Conclusions In conclusion, we found evidence from the HCAHPS survey to demonstrate the negative effects of isolation on patient experience, especially for areas such as communication, staff responsiveness, and likelihood to recommend. Implications for Policy or Practice This work provides support that nurse communication matters a great deal to patients despite their diagnosis, yet this may matter even more in patients, such as those with COVID-19, who are experiencing isolation. The policy implications for nurse staffing are critical for health planners and administrators to consider where there are large numbers of isolation patients to care for. The extra staff time to don and doff personal protective equipment and to provide emotional support in the absence of family members must be considered in planning nurse staffing coverage. 80-R. Using a Measure of Nurse Manager Reasons for Leaving to Inform Role Transformation for the Future Martha Grubaugh, PhD, RN, NE-BC; UCHealth; Aurora, Colorado 10/28/2023, 2:10pm - 3:00pm, Breakout: 2 Background: Nurse managers (NMs) have a pivotal role in cultivating supportive practice environments and ensuring positive patient, nurse, and organizational outcomes. The role of NM is demanding and stressful and it has been exacerbated by the challenges of the COVID-19 pandemic and staffing shortages. Retaining and supporting NMs is essential for ensuring the delivery of high-quality patient care and the overall success of the healthcare organization. Recent national reports indicate that of NMs surveyed, almost 45% either plan to or might leave their position in the next six months. Turnover often creates instability within the organization and leads to disruption in the delivery of care which can negatively impact patient safety, culture, and both financial and organizational outcomes. To help prevent NM turnover, it is important to understand their reason for leaving (RFL) their position, develop RFL response standardization, and a way to measure their RFL. Purpose: The purpose of this research was to develop a structured, quantitative, and parsimonious measure of NM RFL. Methods: A secondary data analysis of quantitative data from a 2017 national NM study was completed. The sample included NMs with inpatient or inpatient/outpatient department responsibilities and intended to leave their position in the next 0-3 years. Demographics and a reason for leaving (RFL) question, with 16 response options, was used as a part of the analysis. Only one response was allowed for the RFL question. (Question: If you plan to leave your current position in the next 0 to 3 years, what is your PRIMARY reason?) Evaluation of all RFL responses was conducted through a review of response frequencies. Responses were categorized based on NM research and a committee of subject matter experts. Results/Outcomes and Implications: There were 181 NMs included in the analysis. The top RFL were: to obtain a promotion or career advancement, retirement, and to obtain different job experience, remaining in nursing. All RFL were able to be grouped into three categories, 1) environmental, 2) personal, and 3) advancement. The categories were then scored as an ordinal measure of decreasing severity, as it relates to a supportive nurse manager practice environment. Environmental reasons=1, personal reasons=2, and professional advancement reasons=3. Of the three developed categories, 19.5% of NMs indicated they left their position due to environmental and personal reasons and 61% left for professional advancement reasons. It is important to consider study implications within the current context and how personal and work-environment stressors from the COVID-19 pandemic effected NM RFL and turnover. Regardless, organizations should focus on interventions related to span of control, work-life balance, and career advancement to frame the NM role for the future. Additional research and development of the RFL measure is needed. It is important to engage NM stakeholders, trend RFL, and test the effectiveness of interventions to proactively address the reasons why NMs leave their position. 82-EBP. Nursing is Not Multiple Choice Mithun Mahinda, CCRN, CMC; UCLA Health; Santa Monica, California 10/29/2023, 12:00pm - 1:50pm, Poster Session A 22-bed critical care unit experienced a 67% drop in retention rates for new hires and nurse residents. Exit interviews of 15 resigning staff members across 3 cohorts during an 18-month period identified dissatisfaction with the unit onboarding and orientation process. Five themes were identified in the exit interviews: lack of standardized education, variations in practice, focus on policies rather than clinical decision-making, lack of clinical skill preparation, and inadequate supplemental educational resources to support learning. Clinical nurse leads identified the need for a comprehensive, standardized, evidence-based practice, and multi-modal educational bundle to improve the onboarding process in order to transition new staff to practice adequately. A literature review demonstrated the best practices to effectively transition clinicians to the bedside focused on instructor teaching strategies, clinical teaching models, and the use of technology. Instructor teaching strategies include the use of evidence-based knowledge dissemination strategies, adequate instructor preparedness, and enhanced communication strategies. The purpose of this initiative was to empower clinical nurse leaders to build a comprehensive, standardized educational bundle to improve staff satisfaction, improve retention, alleviate preceptor burnout, and improve the transition to practice. The PICOT question was as follows: In a critical care unit, how would the use of a comprehensive, standardized, evidence-based practice educational bundle compared to current practice impact staff satisfaction, retention, and preceptor burnout? The theoretical framework used to guide the practice change was the Iowa Model for Evidence-Based Practice. Clinical nurse leaders collaborated with the unit director to identify the need for an educational bundle as a unit priority. An educational team composed of experienced preceptors was formed. The team created an educational program that revolved around critical care principles for seven domains: neurological, respiratory, cardiac, gastrointestinal, genitourinary, hemodynamics, and shock. Education was combined into didactic and simulation courses. Content followed bedside presentation rounds and clinical case scenarios using the Socratic Method. Teaching scripts were created for all instructors to ensure a consistent educational experience. Attendees were given standardized educational tipsheets to study and pre-work prior to educational sessions. Attendees provided feedback after the educational sessions. A pre/post-test was used to assess the impact of educational content on knowledge retention. Instructors were provided with a feedback form to assess their experience with the new format. Since the creation of the education team, we have continued to collect preceptee and preceptor feedback. Preceptee feedback was overwhelmingly positive regarding clinical case scenarios, group discussions, and tipsheets. Preceptors that were instructors of the class for new hires reported feeling prepared to lead their portions and felt the preceptees were more engaged. They noted that they felt a sense of purpose when conducting interactive discussions of clinical case scenarios. The unit's retention rates of new hires and new graduate nurses increased to 79% since the restructure of the new education team aligning with its mission to promote evidenced-based curriculum along with the implementation of the new format of educational resources, classes and standardization. There was a notable knowledge increase from 20-45% across all 7 domains. 83-R. Emergency Preparedness Competency and Training for Nurses: A Scoping Review. Teresa Dodd-Butera, PhD; RN/DABAT; Azusa Pacific University; Azusa, California 10/29/2023, 12:00pm - 1:50pm, Poster Session Emergency Preparedness Competency and Training for Nurses: A Scoping Review. Background/Significance: Nurses comprise the largest sector in the healthcare workforce; and are essential for front line leadership and response during public health emergencies. The COVID-19 pandemic left a heavy burden on the nursing workforce, both physically and mentally. Preparedness and training for nursing students and professional nurses can be part of an overall strategy for community and workforce readiness. Objective: The objective of this scoping review was to identify evidence of emergency preparedness training programs for future and current professional nurses. Methods: This research used the Joanna Briggs Institute (JBI) scoping review methodology following steps of PRISMA Extension for Scoping Reviews (PRISMA-ScR) 2020. A comprehensive search was limited to the emergency preparedness training of nurses and nursing students, peer-reviewed, full text articles, in the English language, published from January 1, 2017 to December 31, 2022 through Ebsco and Proquest databases. Results: A total of 597 relevant articles were identified from 200 different journals and from different countries from all five continents (America, Europe, Asia, Australia, and Africa). Five main categories of evidence were identified including training for professional nurses in the work setting, integration into curriculum for nursing students, components of emergency preparedness training programs, personal health and leadership development during emergencies, and collaboration with different healthcare professionals and stakeholders during disasters. Implications: Findings indicate a critical need to develop emergency preparedness training programs for nurses and nursing students. This can be achieved through continuing education, curriculum development at all levels of nursing education, and nursing leadership. Equitable community readiness is dependent on workforce competency, advocacy, and leadership by all nurses for protection and preparation during the next public health emergency. 84-EBP. Assessing the Effectiveness of the University of Alabama Birmingham. STEMI Program: A Program Evaluation of Performance Measures and Outcomes for UAB STEMI Patients Sherri Wall, MSHA BSN RN CNOR; UAB School of Nursing; Birmingham, Alabama 10/29/2023, 12:00pm - 1:50pm, Poster Session Assessing the Effectiveness of the University of Alabama Birmingham (UAB) ST Elevation Myocardial Infarction (STEMI) Program: A Program Evaluation of Performance Measures and Outcomes for UAB STEMI patients. S. Wall, S. Miltner, M. Goolsby, E. Pentecost, A. Reed. M. Hammett, T. Poe, G. Eagerton April 25, 2023 Abstract The UAB STEMI program provides state of the art care using evidence-based guidelines to improve outcomes for patients experiencing STEMI. Coordination between emergency medical services (EMS), referring hospitals, UAB Cath Lab Staff, and the UAB hospital system is required to ensure rapid and efficient diagnosis and treatment of STEMI patients. The purpose of this evaluation is to assess the effectiveness of the UAB STEMI program. Methods: This DNP project will utilize the CDC Six Steps Program Evaluation Framework to evaluate the organization’s ability to provide the highest standard of care for STEMI Patients. A retrospective analysis of data will be collected from patients with STEMI who were treated at UAB Heart and Vascular Center between January 2020 and December 2022. Data will be obtained from the UAB STEMI database Get With The Guidelines (GWTG), and Cath PCI. The primary outcomes measures in this evaluation include time from first medical contact to PCI treatment, door-to-balloon times, ECG within 10 minutes of arrival and the in-hospital STEMI patient diagnosis to PCI treatment. Outcomes: 457 UAB patients with STEMI will be included in this program evaluation. Data analysis will consist of descriptive statistics: assessing median, Shewhart Statistical Process Control (SPC) charts to evaluate the performance over time and identify positive and negative trends. This project will start upon ethical approval May 2023. Discussion: Evidence reflects STEMI patients who receive reperfusion of the coronary 90 minutes experience greater chance of survival. The program evaluation will evaluate UAB STEMI Program’s outcomes and performance for the STEMI patient. The evaluation will identify opportunities for improvements and make recommendations from evidence-based practice for future performance. 85-R. System Chief Nurse Executive’s Leadership Practices to Support, Mentor, Develop and Retain Nurse Leaders Kenneth David Bailey, PhD, MBA, RN, CCRN-K, NEA-BC, FACHE, FAAN; UCLA Health - Santa Monica Medical Center; Santa Monica, California 10/29/2023, 11:10am - 12:00pm, Breakout: 12 In 2019, the National Academy of Science identified clinician burnout as a growing public health concern. The COVID-19 pandemic has only compounded this crisis and transformed it into an escalating fracture within our healthcare system. Concurrently evolving with this emergency is a rise in the intent to leave nurses from the profession. Frontline nurse leaders (FNLs) are the lynchpin in ensuring healthcare systems function. FNLs have accountability over patient care and clinician well-being. Focused effort must be directed toward addressing clinician burnout. However, without addressing the well-being of FNLs, the fault line in our healthcare system becomes a wide chasm. Recently, published literature began to emerge that both describe and address frontline clinician burnout. Unfortunately, very few, if any address issues related to leaders. |
Time(Central) |
Sunday, Oct 29 |
Location |
| 7:30am - 8:45am |
Breakfast (open to all attendees) |
2nd Floor Foyer |
| 7:30am - 5:30pm |
Exhibit Area |
2nd Floor Foyer |
| 8am - 3:15pm |
Registration | 2nd Floor Foyer |
| 9am - 10am |
Keynote Address Nursing Leadership for Inclusive Excellence
In recent years, organizations have been making more intentional efforts to advance diversity, equity, inclusion, and belonging (DEIB). Despite the increased focus on DEI, many leaders struggle with cultivating belonging on their teams. In this session, we will explore how nursing leaders can leverage principles of inclusive leadership to create environments where all members of their organizations can experience belonging and thrive. Learner Objectives:
|
Wynfrey ABC |
| 10:10am - 11:00am |
Breakout 7 78-R. Mentoring clinical nurses with new approaches
Learner Objectives:
56-R. Nurses’ fatigue and sleep quality and perception of the night shift work environment
Learner Objectives:
|
Riverchase A |
| 10:10am - 11:00am |
Breakout 8 49-EBP. A Nurse Leader Guide to Building an Equitable and Inclusive Nursing System Float Team: Increasing Self-Reliance and Financial Sustainability
Learner Objectives:
14-QI. Utilizing the Nursing Leadership Mission Critical Checklist ©: A Pilot Project
Learner Objectives:
|
Riverchase B |
| 10:10am - 11:00am |
Breakout 9 24-R. Modern Perceptions of Leadership as an Influential Factor in Nursing Retention: A Phenomenological Study
Learner Objectives:
44-R. Generation Z nurses bring a new generation of diversity and passion to nursing!
Learner Objectives:
|
Wynfrey DE |
| 11:10am - 12:00pm |
Breakout 10 15-R. COVID-19 Pandemic and New Nurses’ Transition to Practice Outcomes: A Multi-site, Longitudinal Study
Learner Objectives:
45-R. Early Wins: Preliminary Results of the Workforce Engagement for Compassionate Advocacy, Resilience, and Empowerment (WE CARE) intervention for Improving Nurse Well-Being
Learner Objectives:
|
Riverchase A |
| 11:10am - 12:00pm |
Breakout 11 39-R. Nurse Faculty Perceptions of Leadership Behaviors that Impact Job Satisfaction: Creating an Equitable and Inclusive Nurse Faculty Future
Learner Objectives:
66-ASP. Financial Toxicity: The Importance of Understanding the Cost of Health Care
Learner Objectives:
|
Riverchase B |
| 11:10am - 12:00pm |
Breakout 12 85-R. System Chief Nurse Executive’s Leadership Practices to Support, Mentor, Develop and Retain Nurse Leaders
Learner Objectives:
33-R. The COVID-19 Pandemic: Exploration of Nurse Leaders’ Experiences Managing the Clinical Environment during a Crisis
Learner Objectives:
|
Wynfrey DE |
| 12pm - 1:50pm |
Lunch & Poster Showcase (see poster tab) (open to all attendees) |
2nd Floor Foyer |
| 2:00pm - 2:50pm |
Breakout 13 19-ASP. Sustainable Funding in Leadership Science
Learner Objectives:
55-ASP. A Strong Nurse Academic Service Partnership Advances Professional Nursing and Creates Positive Outcomes
Learner Objectives:
|
Riverchase A |
| 2:00pm - 2:50pm |
Breakout 14 75-R. Educational Pathways of Nurse Practitioners who work in Emergency as Predictors of Competence and Capability
Learner Objectives:
61-R. Burnout Syndrome in Nursing Technicians in Intensive Care: the impact of the Covid-19 Pandemic
Learner Objectives:
|
Riverchase B |
| 2:00pm - 2:50pm |
Breakout 15 25-EBP. The Hospital-Based Nurse Scientist as A Senior Nurse Leader: Evidence to Support the Role
Learner Objectives:
20-EBP. Nursing Leadership Development: Recommendations from A Systematic Review
Learner Objectives:
|
Wynfrey DE |
| 3:00pm - 3:50pm |
Breakout 16 6-R. Impact of the Doctor of Nursing Practice Degree: A Look Back from the Beginning of the First DNP Program to Today
Learner Objectives:
50-R. Critical Factors for Success in Advising Doctor of Nursing Practice Students: Creating Curious, Inclusive Nursing Leaders of the Future- It’s Not Just About the Project
Learner Objectives:
|
Riverchase A |
| 3:00pm - 3:50pm |
Breakout 17 30-R. Leveraging Social Media to Create an Equitable and Inclusive Future for the Nursing Workforce
Learner Objectives:
51-R. The Role of Cultural Self-Efficacy with Nurse Leaders in Promoting an Inclusive Classroom Environment
Learner Objectives:
|
Riverchase B |
| 3:00pm - 3:50pm |
Breakout 18 69-EBP. Building Nurse Entrepreneurs for an Equitable Future
Learner Objectives:
74-QI. Staffing by Acuity – Myth or Reality? Program evaluation of an EHR imbedded Nursing Workload Acuity Tool using ANA’s Principles for Nurse Staffing
Learner Objectives:
|
Wynfrey DE |
| 4pm - 5:30pm |
ALSN Membership Meeting & Awards with Wine & Cheese (ALSN members only) |
Wynfrey ABC |
| 5:30pm |
Dinner on your own |
Time(Central) |
Monday, Oct 30 |
Location |
| 7:30am - 8:45am |
Breakfast (open to all attendees) |
2nd Level Foyer |
| 7:30am - 12pm |
Exhibit Area |
2nd Level Foyer |
| 9am - 10:30am |
International Keynote Panel Global Community Imbalance: International Dilemmas and Ethical Struggle with DEI This panel presentation will feature global leaders in nursing discussing ways to build a global community while simultaneously addressing cultural humility and ethical accountability. Moderator:
Panelists:
Learner Objectives:
|
Wynfrey ABC |
| 10:35am - 11:30am |
Breakout 19 68-R. Examining the role of nursing leadership in Brazilian university hospitals in the COVID-19 crisis
Learner Objectives:
18-R. Voices of International Nursing Students enrolled in a nursing program in the United States
Learner Objectives:
|
Riverchase A |
| 10:35am - 11:30am |
Breakout 20 67-R. A Pathway for Gender Equity in Healthcare: Solutions for Health Leaders
Learner Objectives:
36-QI. Improving outcomes for advanced heart failure patients using a nurse-lead quality improvement program in Brazil
Learner Objectives:
|
Riverchase B |











 Next Generation Leaders: Leadership Through the Lens of Social and Organizational Justice
Next Generation Leaders: Leadership Through the Lens of Social and Organizational Justice